
Perimenopause, Explained: Symptoms, Causes, and a Practical Roadmap to Lasting Relief
Perimenopause is the transition leading into menopause when reproductive hormones become unpredictable, producing physical, emotional, and cognitive symptoms that can interfere with everyday life. Most people assigned female at birth experience this change in their 40s, though it can start earlier or later depending on genetics, surgeries, or lifestyle. This guide outlines the biology behind perimenopause, connects common symptoms to likely causes, and provides a practical, evidence-informed plan for relief — from lifestyle and natural approaches to targeted medical options like bioidentical hormone replacement therapy (BHRT). You’ll learn how hormone swings cause hot flashes and mood shifts, when testing is useful, and how integrative therapies (including supervised detox and IV nutrient support) can support recovery. The article is organized for clarity: definitions and mechanisms, a symptom-to-root-cause map, BHRT basics and safety, natural and integrative options, the value of a personalized root-cause approach, and concise FAQs to help you act with confidence.
What Is Perimenopause and How Does It Affect Hormone Balance?
Perimenopause is the biological transition before menopause marked by changing ovarian function that shifts levels of estrogen, progesterone, and other sex steroids. Those changes can cause menstrual irregularities and altered temperature regulation. As ovarian follicles decline and ovulation becomes less consistent, progesterone production drops while estrogen becomes more variable — sometimes surging, often trending down — and pituitary hormones FSH and LH rise in response. These hormonal dynamics influence brain chemistry, blood vessel tone, sleep patterns, and genital tissues, turning endocrine shifts into the symptoms described below. Understanding these mechanisms helps guide therapies that stabilize hormones, support metabolic resilience, and identify co‑drivers like thyroid or adrenal issues. The following subsections outline typical hormonal patterns and timelines so you can recognize the physiologic signals of the transition.
What Are the Hormonal Changes During Perimenopause?
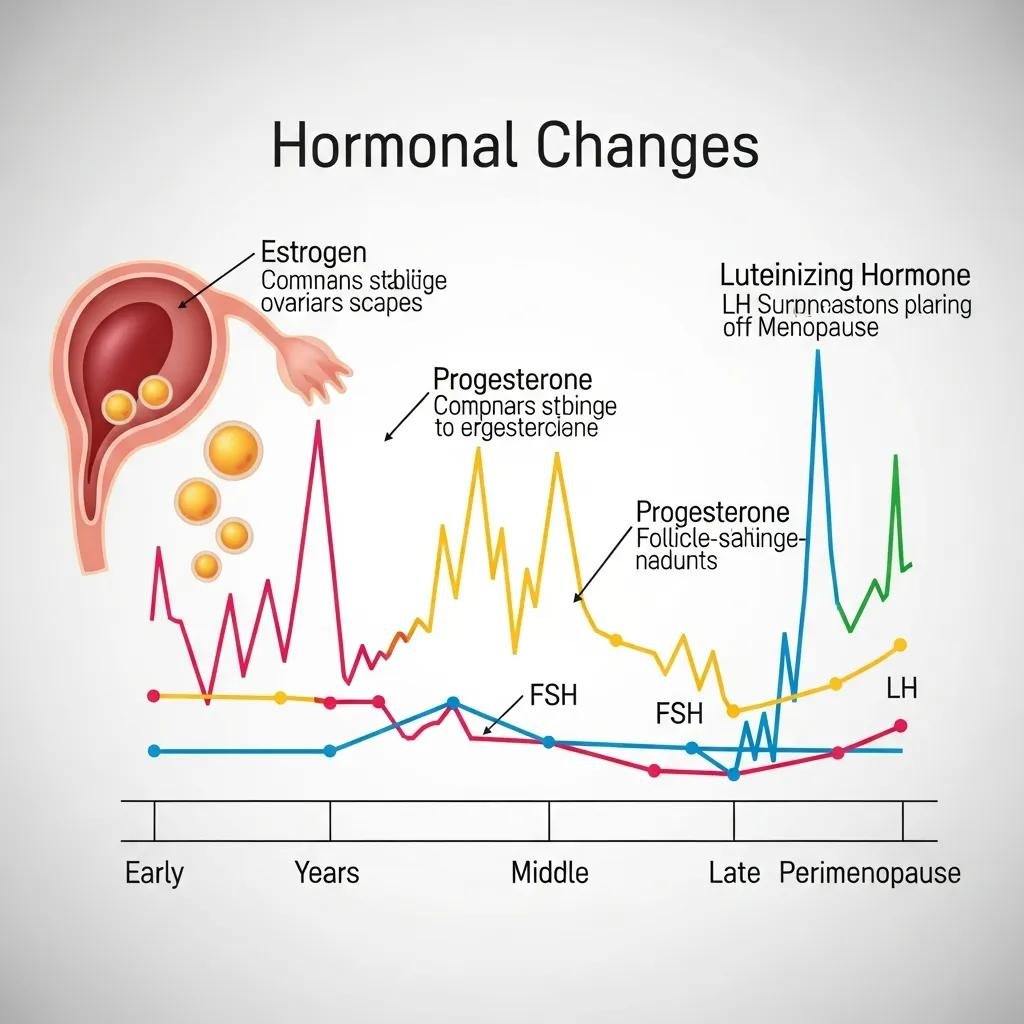
Perimenopause commonly shows three hormonal patterns: inconsistent estrogen production, declining progesterone from fewer ovulatory cycles, and relative shifts in androgens such as testosterone. As follicles thin out, estradiol can spike unpredictably — which may cause heavy or irregular bleeding — yet overall estrogen often trends downward over time. Progesterone falls because anovulatory cycles and luteal phase problems become more frequent, contributing to sleep disruption, mood swings, and PMS‑like symptoms. Clinically, FSH often rises while estradiol measurements vary, so a single lab value can be misleading; tracking symptoms alongside trends gives a clearer picture. These endocrine shifts interact with thyroid and adrenal function, so a systems-based assessment is frequently helpful when interpreting labs and planning treatment.
How Long Does the Perimenopause Transition Typically Last?
Perimenopause duration ranges widely — from several months to a number of years — most commonly about 4–8 years. Individual timelines depend on genetics, smoking, prior ovarian surgery, chemotherapy or radiation, and body composition. Those with ovarian removal or certain medical treatments may go through a faster transition, while higher BMI and some endocrine conditions can change symptom timing and intensity. Clinicians prioritize symptom patterns and functional impact over strict age cutoffs; persistent disruptive symptoms or sudden changes deserve evaluation. Tracking menstrual cycles, hot flash frequency, sleep quality, and mood over several months creates the context needed for appropriate testing and a tailored care plan.
What Are the Common Symptoms of Perimenopause and Their Root Causes?
Perimenopause most often brings vasomotor symptoms, menstrual changes, genitourinary issues, mood and cognitive symptoms, and metabolic shifts — each linked to specific hormonal and systemic drivers. A root-cause framework helps separate direct effects of estrogen and progesterone imbalance from contributing factors like adrenal dysregulation, thyroid disease, nutrient shortfalls, chronic inflammation, or toxin exposure. Clinicians use this mapping to prioritize tests and treatments that address drivers rather than only masking symptoms. Below we list hallmark complaints and then show a concise table linking symptoms to likely causes and practical interventions to guide decision-making.
Which Physical and Emotional Symptoms Indicate Perimenopause?
Common physical signs include irregular or heavier periods, hot flashes and night sweats, fragmented sleep, vaginal dryness and sexual changes, and shifts toward central weight gain. Emotional and cognitive symptoms often include mood swings, increased anxiety, low mood or depression, memory slips or “brain fog,” and lower stress tolerance. Severity varies: vasomotor symptoms tend to peak in late perimenopause, while genitourinary changes often worsen as estrogen falls. Red flags — very heavy bleeding, severe depression, sudden sharp pelvic pain, or signs of cardiovascular or thrombotic events — need immediate medical attention. Recognizing symptom clusters helps focus evaluation and speed effective treatment.
Different symptoms commonly reflect distinct physiologic drivers:
- Hot flashes: estrogen variability disrupting hypothalamic temperature control.
- Irregular bleeding: anovulation and luteal phase insufficiency.
- Vaginal dryness: local estrogen deficiency leading to tissue thinning.
- Mood changes: progesterone withdrawal and shifts in neurotransmitters.
- Cognitive issues: poor sleep plus estrogen-related neurotransmitter changes.
That symptom patterning guides targeted testing and personalized treatment choices discussed next.
Here’s a short summary of common symptom groups:
- Vasomotor & sleep: hot flashes, night sweats, insomnia, fragmented sleep.
- Reproductive changes: irregular cycles, heavier or lighter bleeding, unpredictable flow.
- Genitourinary: vaginal dryness, painful intercourse (dyspareunia), urinary urgency or recurrent infections.
- Neurocognitive & mood: mood swings, anxiety, depression, brain fog, memory lapses.
These categories help prioritize which hormonal or integrative strategies are most likely to bring relief.
Intro to EAV table: The table below links common symptoms to likely root causes and practical interventions, blending conventional and integrative options.
| Symptom | Possible Root Causes | Intervention | Evidence / Notes |
|---|---|---|---|
| Hot flashes / night sweats | Estrogen fluctuation; hypothalamic dysregulation | Hormone stabilization (estrogen ± progestogen); cooling strategies; SSRI/SNRI if needed | Strong evidence for estrogen; nonhormonal options can help |
| Irregular bleeding | Anovulatory cycles; luteal insufficiency; fibroids | Cycle tracking; progesterone support; imaging when bleeding is heavy | Investigate structural causes if bleeding is significant |
| Vaginal dryness / dyspareunia | Local estrogen deficiency; vaginal atrophy | Local vaginal estrogen, moisturizers, pelvic floor therapy | Local treatments work well with minimal systemic exposure |
| Mood swings / anxiety | Progesterone decline; neurotransmitter shifts; stress | Psychotherapy, lifestyle changes, consider BHRT, SSRI if indicated | Often multifactorial—best treated with combined approaches |
| Sleep disturbance / brain fog | Hormone changes + hot flashes + stress | Sleep hygiene, CBT‑I, treat vasomotor symptoms, consider BHRT | Improving sleep often improves cognition |
| Weight gain / metabolic shift | Estrogen decline, insulin resistance, reduced muscle mass | Nutrition plan, resistance training, metabolic assessment | Lifestyle changes are foundational; evaluate endocrine contributors |
Summary: Mapping symptoms to causes clarifies that effective perimenopause care blends hormone-targeted therapies with lifestyle, behavioral, and root‑cause interventions — a systems view that supports personalized plans rather than one-size-fits-all fixes. Next, we explain how BHRT fits into an individualized strategy.
How Can Bioidentical Hormone Replacement Therapy Help Manage Perimenopause?
Bioidentical hormone replacement therapy (BHRT) uses hormones chemically identical to the body’s natural steroids to reduce hot flashes, stabilize menstrual irregularity, improve sleep and mood, and treat genitourinary atrophy when appropriate. Compared with older regimens, BHRT often focuses on estradiol and micronized progesterone or delivery forms that better mimic physiology. Personalization involves symptom-guided dose adjustments and, when appropriate, periodic labs and clinical monitoring to balance benefit and safety. Many patients notice quick reductions in hot flashes, better sleep, and more predictable cycles; safety discussion includes individualized assessment of thromboembolism risk, breast cancer history, and cardiovascular factors. Choosing BHRT should be a shared decision that weighs symptom burden, personal risk, and nonhormonal options. The sections below outline personalization and monitoring to help guide conversations with your clinician.
What Is Bioidentical Hormone Replacement Therapy and How Is It Personalized?
Personalizing BHRT starts with a detailed history, symptom mapping, and selective labs to assess estrogen, progesterone, and androgen status along with thyroid and metabolic measures. Common delivery options include transdermal estradiol patches or gels, oral or micronized progesterone, and either standardized or compounded preparations chosen for absorption, convenience, and risk profile. Dosing is adjusted based on symptom response and tolerability, with follow-up visits to tweak route or amount and to monitor blood pressure and metabolic markers. Personalization also takes into account lifestyle, fertility goals, and coexisting conditions; the aim is to restore balance while minimizing side effects through careful follow-up and evidence-based protocols.
Below is a comparison-style table summarizing common BHRT approaches.
| Therapy Type | Personalization Attribute | Typical Outcome / Considerations |
|---|---|---|
| Transdermal estradiol | Steady systemic absorption; dose adjusted by symptom relief | Less hepatic first-pass effect; generally favorable metabolic profile |
| Oral estradiol | Convenient dosing; influenced by liver metabolism | Can affect clotting factors; monitor lipids and liver tests |
| Micronized progesterone | Often improves sleep; used cyclically or continuously | Helps control bleeding and protects the endometrium |
| Compounded BHRT | Custom combinations and doses | Requires strict compounding standards and close monitoring |
Summary: Thoughtful BHRT personalization improves symptom relief and safety by matching formulation, route, and dose to each person’s physiology. Ongoing monitoring and multidisciplinary care help guide safe adjustments. Below is a brief note about how our clinic approaches BHRT.
Integration paragraph (practice mention, brief): At Internal Healing and Wellness MD, Dr. Fred Bloem prioritizes individualized BHRT plans that begin with a thorough intake and include follow-up visits to titrate therapy and track outcomes. New patients are invited to discuss a personalized BHRT strategy during consultation to determine the best formulation and monitoring plan for their needs.
What Natural and Integrative Therapies Support Perimenopause Wellness?

Natural and integrative therapies can complement medical care by supporting detox pathways, correcting nutrient gaps, improving sleep and stress resilience, and strengthening metabolic health — all factors that influence symptom severity and recovery. Evidence supports strategies such as phytoestrogen‑rich foods, cognitive behavioral therapy for insomnia, and exercise (particularly resistance training) to preserve muscle. Certain supplements — for example vitamin D and magnesium when deficient — can help. Integrative services used in supervised settings, like IV nutrient therapy or carefully planned detox protocols, aim to replenish cofactors for hormone metabolism and reduce toxin burdens that may interfere with endocrine signaling. These adjuncts are intended to support, not replace, core hormonal and lifestyle therapies. The next sections explain how detox and IV therapies may support hormonal balance and list practical lifestyle steps you can start today.
How Do Detoxification and IV Therapies Aid Hormonal Balance?
Detox and IV nutrient therapies are designed to support liver phase I/II pathways, restore micronutrients needed for steroid metabolism, and correct deficits that sap energy and concentration. Common IV formulations in integrative care include antioxidant blends (such as glutathione) and nutrient cocktails aimed at mitochondrial support and reducing oxidative stress; when given under medical supervision, these therapies can rapidly raise nutrient levels and ease symptoms like fatigue or brain fog. Detox programs focus on improving hepatic conjugation through diet changes, targeted supplements, and lifestyle adjustments that reduce exposure to endocrine-disrupting chemicals. Safety and clinical oversight are essential: IV and detox plans should be individualized, and protocols must account for overall health to prevent symptom flares. The next subsection offers nutrition and lifestyle actions you can implement immediately.
Common IV/detox adjuncts used in integrative perimenopause care include:
- Antioxidant IVs: to reduce oxidative stress and support mitochondria.
- Glutathione-based therapies: to bolster detox pathways and cellular protection.
- Nutrient repletion IVs: B vitamins, magnesium, and trace minerals to restore energy and mood.
Intro to EAV table: The table below compares integrative therapy options, the symptoms they target, and typical frequency or expected benefits to help you decide what might fit your plan.
| Therapy | Targeted Symptoms / Mechanism | Typical Frequency / Expected Benefit |
|---|---|---|
| IV nutrient cocktails | Fatigue, brain fog; replenish B vitamins and minerals | Often monthly to biweekly initially; energy improvements within days |
| Glutathione IV | Oxidative stress, support for detox pathways | Series of 4–6 sessions commonly; supports hepatic detoxification |
| Supervised detox protocols | Toxin burdens that may affect hormones | Short-term medically guided programs; gradual symptom improvement |
| Oral nutraceuticals | Sleep, mood, vasomotor symptoms | Daily use; benefits typically appear over weeks to months |
Summary: Integrative therapies can support metabolic and detox pathways that influence hormone function, but they work best when integrated with hormone care and lifestyle changes and delivered under clinical supervision to ensure safety and effectiveness. Next, we cover practical nutritional and lifestyle measures that form the foundation of symptom control.
Which Nutritional and Lifestyle Strategies Help Manage Symptoms Naturally?
Natural symptom management focuses on eating patterns that stabilize blood sugar, support liver conjugation pathways, and supply phytoestrogens and cofactors for hormone synthesis. Key priorities include consistent protein at meals, fiber‑rich whole foods, anti‑inflammatory fats (or oily fish/omega‑3s), and culturally appropriate phytoestrogen sources such as soy. Exercise should combine aerobic activity with resistance training to preserve lean mass and metabolic health. Address sleep with good hygiene and CBT‑I techniques, and reduce stress with mindfulness, breathwork, or cognitive behavioral strategies to lower adrenal overactivity. Supplements should be tailored to testing — common considerations are vitamin D, magnesium glycinate, and omega‑3s — and used under professional guidance to manage dosing and interactions.
Practical lifestyle priorities:
- Nutrition: emphasize protein, fiber, and anti‑inflammatory fats to stabilize insulin and support the liver.
- Exercise: combine resistance training with aerobic activity to maintain muscle and metabolic function.
- Sleep & stress: establish sleep routines and evidence‑based stress management to reduce symptom amplification.
Summary: These lifestyle pillars reduce symptom severity and boost the effectiveness of medical treatments by addressing core metabolic and inflammatory drivers. When integrated with targeted medical and integrative therapies, they increase the likelihood of lasting relief.
Integration paragraph (practice mention, brief): Internal Healing and Wellness MD uses supervised IV nutrient protocols and individualized detox plans as adjuncts to lifestyle changes and BHRT when clinically appropriate, applying an integrative model to optimize hormone balance and symptom recovery.
How Does a Personalized Holistic Approach Improve Perimenopause Management?
A personalized holistic plan uses root-cause analysis to identify contributors beyond ovarian hormone changes — things like thyroid imbalance, adrenal stress, gut dysfunction, nutrient shortfalls, or toxin exposures — then sequences interventions to address those drivers and rebuild resilience. The process begins with a comprehensive intake, targeted laboratory testing, and functional assessments to prioritize actions that will yield the biggest clinical benefit. Individualized care typically combines evidence‑based BHRT where indicated, metabolic and nutritional optimization, behavioral interventions for sleep and mood, and integrative adjuncts such as IV therapy or detox when helpful. Regular outcome tracking with symptom scales and objective labs lets clinicians refine the plan over time, improving the chances of meaningful, durable improvement.
Why Is Root Cause Analysis Essential in Treating Perimenopause Symptoms?
Root cause analysis moves care from simply masking symptoms to addressing upstream drivers that maintain them. Examples include undiagnosed hypothyroidism producing fatigue, chronic stress increasing cortisol and worsening insomnia, or heavy metal burden impairing steroid metabolism. Targeted testing — thyroid panels, adrenal assessments, metabolic labs, and selective toxin screens — helps prioritize treatments and avoid unnecessary or ineffective interventions. Treating drivers can lower the hormone doses needed and improve response to BHRT, while ongoing monitoring helps identify contraindications or comorbidities early. This systems-based approach tends to produce more durable symptom control and empowers patients to take an active role in recovery.
How Does Dr. Fred Bloem’s Integrative Care Empower Patients?
Dr. Fred Bloem’s model prioritizes longer visits for a thorough assessment, patient education, and shared decision-making that produces individualized protocols combining BHRT, nutrition, IV therapies, and lifestyle coaching. A typical pathway includes an initial visit to map symptoms and drivers, targeted testing to refine the plan, a personalized treatment protocol with scheduled follow-ups, and measurable goals for symptom reduction and functional recovery. Patients are taught self-monitoring strategies, practical lifestyle steps, and clear milestones for adjusting therapy — an approach that supports adherence and long-term success. For those seeking care, the practice offers integrative evaluations to design safe, effective plans aligned with each person’s goals.
Business-integration list (brief introduction and summary): Core elements of the practice workflow used to personalize care include:
- Assessment: extended intake and driver-focused testing to inform treatment choices.
- Personalized plan: a tailored mix of BHRT, lifestyle change, and integrative adjuncts.
- Follow-up: scheduled visits for dose titration, monitoring, and outcome measurement.
Summary: This structured pathway helps people move from feeling overwhelmed by symptoms to clear, achievable treatment goals — while preserving education, collaboration, and safety at every step.
Frequently Asked Questions
What lifestyle changes can help alleviate perimenopause symptoms?
Targeted lifestyle changes can meaningfully reduce perimenopause symptoms. Focus on a whole‑food diet with consistent protein, healthy fats, and fiber to stabilize blood sugar. Regular exercise — including resistance work and aerobic activity — supports muscle and metabolic health. Practice good sleep hygiene and consider CBT‑I for persistent insomnia. Stress‑reduction tools like mindfulness, breathwork, and therapy help manage anxiety and mood. These approaches work best alongside medical care when needed.
How can I track my symptoms effectively during perimenopause?
Tracking is key to spotting patterns and guiding treatment. Use a simple journal or an app to log cycle changes, hot flash frequency and intensity, mood shifts, and sleep quality. Record how symptoms affect daily activities. Share at least three months of data with your clinician to build a reliable picture for testing and treatment decisions.
Are there specific supplements recommended for perimenopause management?
Supplements can help when chosen based on individual needs. Commonly considered options include vitamin D for bone health, magnesium for sleep and mood support, and omega‑3s for inflammation control. Phytoestrogen foods like soy may offer mild estrogenic effects in culturally appropriate amounts. Always consult a healthcare provider before starting supplements to ensure they’re safe and suitable for your history and medications.
What role does stress play in perimenopause symptoms?
Stress can worsen perimenopause symptoms by raising cortisol and disrupting sleep, mood, and energy. Chronic stress may also encourage unhealthy coping behaviors that compound symptoms. Regular stress management — mindfulness, yoga, therapy, or structured relaxation — helps lower cortisol, improve sleep, and lessen symptom burden.
When should I seek medical advice regarding my perimenopause symptoms?
Seek medical care if symptoms are severe, rapidly worsening, or interfering with daily life — for example, very heavy bleeding, intense mood changes, or major sleep loss. New, concerning signs such as severe pelvic pain or cardiovascular symptoms also call for prompt evaluation. Regular check-ins let clinicians monitor progress and adjust treatment safely.
Can perimenopause affect my sexual health?
Yes. Hormonal changes can cause vaginal dryness, decreased libido, and discomfort during sex due to lower estrogen and vaginal thinning. Open communication with partners and your clinician is important. Effective options include vaginal moisturizers, lubricants, pelvic floor therapy, and local or systemic hormone treatments tailored to your needs.
What Are the First Signs of Perimenopause?
Early signs often include changes in menstrual regularity (cycles shorter or longer than usual), occasional hot flashes or night sweats, new sleep problems, and intermittent mood shifts. Track cycles and symptoms for about three months to provide useful pattern data for assessment. Mild symptoms may respond to lifestyle changes and basic labs; severe or rapidly worsening problems — especially very heavy bleeding or significant depression — should prompt prompt medical evaluation. Start by documenting frequency, severity, and the effect on daily function to guide shared decision‑making.
Can Perimenopause Cause Anxiety and Depression?
Yes. Hormone fluctuations — especially progesterone withdrawal and estrogen variability — can affect neurotransmitters and increase vulnerability to anxiety and depression. Poor sleep and life stressors make this more likely. Treatment combines psychotherapy (including CBT), sleep and lifestyle measures, and medical options like BHRT or targeted medications when indicated. Seek urgent care for suicidal thoughts, severe impairment, or sudden mood deterioration. Integrated plans addressing sleep, hormones, and psychosocial supports achieve the best results.
What Are the Best Natural Ways to Manage Perimenopause Symptoms?
Top natural strategies include stabilizing blood sugar with balanced meals, increasing omega‑3 and fiber intake, maintaining regular resistance and aerobic exercise, practicing sleep hygiene and CBT‑I techniques, and using stress‑reduction tools such as mindfulness or structured therapy. Supplements like vitamin D, magnesium, and targeted phytoestrogens may help when selected based on testing. If symptoms persist despite lifestyle measures, discuss medical options such as BHRT with your clinician. Combining natural strategies with medical oversight maximizes symptom control while minimizing risk.
How Does Hormonal Birth Control Affect Perimenopause Symptoms?
Hormonal contraceptives can regulate bleeding and sometimes ease vasomotor symptoms, but they may mask the natural transition and complicate interpretation of ovarian function tests. Whether to continue or stop contraception in perimenopause depends on symptom control, cardiovascular risk, and fertility goals. Clinicians often plan a supervised transition off hormonal birth control with symptom tracking and appropriate testing to determine next steps.
Final Call to Action paragraph (business-focused, brief): If perimenopause symptoms are disrupting your life and you want a personalized, integrative plan, Internal Healing and Wellness MD — led by Dr. Fred Bloem — offers thorough evaluations combining root‑cause analysis, individualized BHRT, IV nutrient support, and lifestyle coaching. To explore a tailored plan, call (301) 260-2601 or visit us at 10400 Connecticut Ave Ste 206, Kensington MD 20895-3941 to schedule a consultation and begin a structured path toward lasting relief.
Conclusion
Knowing how perimenopause affects your body and mind gives you tools to take control during this transition. A personalized approach — blending lifestyle changes, targeted medical care, and thoughtful integrative support — can deliver meaningful, lasting relief. If you’re ready to explore a plan tailored to your goals and health history, contact our team for a comprehensive evaluation. Together we’ll create a path that prioritizes your well‑being and quality of life.



