Exosome Therapy for Tendon & Ligament Repair

Harness the Power of Exosomes for Tendon & Ligament Repair
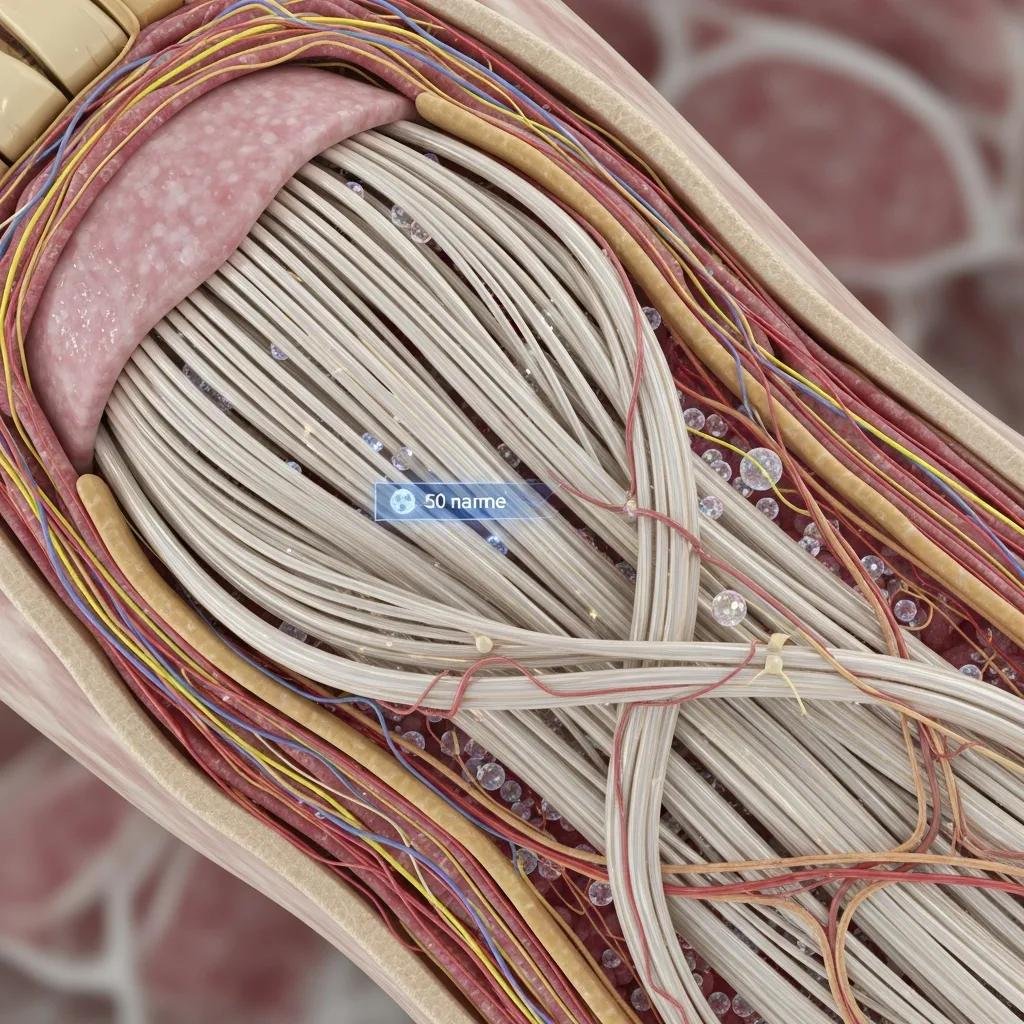
Exosome therapy uses tiny, cell‑derived extracellular vesicles to deliver concentrated regenerative signals that reduce inflammation and encourage tissue remodeling in injured tendons and ligaments. This article describes how exosomes work as a cell‑free regenerative option, which tendon and ligament problems commonly benefit, how the injections are performed, and how results compare with PRP and stem‑cell approaches. Many patients want non‑operative choices to ease pain, restore function, and avoid surgical downtime — exosome therapy offers targeted biological cues to shift the healing environment and support collagen repair and new blood‑vessel growth.
Below we review mechanisms of action, condition‑specific use, patient pathways and recovery timelines, practical comparisons with other biologics, common patient questions, and what to expect when receiving exosome therapy at an integrative clinic.
Throughout, we highlight current research perspectives, realistic timelines for improvement, and practical considerations for choosing the most appropriate regenerative strategy.
What is Exosome Therapy and How Does It Support Tendon and Ligament Healing?
Exosome therapy is a cell‑free regenerative approach that delivers extracellular vesicles loaded with proteins, RNAs, and growth factors to change local cellular behavior and promote repair. These vesicles act as biological messengers that quiet pro‑inflammatory signals, encourage macrophages to adopt a repair‑oriented phenotype, and stimulate resident fibroblasts to make and reorganize collagen. Clinically this can translate to less pain, faster matrix remodeling, and stronger tendons or ligaments — often allowing an earlier, safer return to activity. Understanding these mechanisms helps clinicians decide when exosomes are the right option versus other biologic or surgical treatments.
Exosome actions can be grouped into a few practical, clinically relevant processes:
- Delivery of growth factors and signaling RNAs that stimulate collagen production and local cell proliferation.
- Immune modulation by shifting macrophages from a pro‑inflammatory to a pro‑regenerative state.
- Promotion of angiogenesis and improved local blood flow to support sustained tissue repair.
These mechanisms explain improved matrix quality and symptom relief, and they guide clinical decision‑making about candidate selection and outcome measurement.
What are Exosomes and Why Do They Matter in Regenerative Care?
Exosomes are nanoscale extracellular vesicles released by many cell types that carry concentrated cargo — proteins, lipids, messenger RNAs and microRNAs — used in intercellular communication. As a therapeutic product, exosomes offer a cell‑free way to deliver reparative signals without transferring living donor cells, which reduces certain safety and regulatory complexities linked to cell‑based therapies. Their small size helps them penetrate tissue and be taken up by local cells, allowing focused modulation of inflammation and activation of intrinsic repair processes. Recent studies position exosomes as a versatile platform for delivering growth factors and genetic regulators that accelerate extracellular matrix remodeling in injured soft tissues.
Because exosomes lack viable donor cells, they are often viewed as lower risk for immune incompatibility and tumorigenic potential compared with some cell therapies. That cell‑free profile is one reason clinicians consider exosomes when stimulating the body’s own repair machinery is preferred over implanting cells.
How Do Exosomes Reduce Inflammation and Stimulate Tissue Repair?
Exosome cargo contains signaling molecules that influence both immune and structural cells in tendons and ligaments. These signals can suppress pro‑inflammatory cytokines and increase anti‑inflammatory mediators. In injured tissue, exosomes help polarize macrophages toward an M2‑like, pro‑repair phenotype, reducing chronic inflammation and creating a microenvironment that supports healing. At the same time, exosome signals encourage tenocytes and ligament fibroblasts to increase collagen type I production and reorganize the extracellular matrix, improving tensile strength and functional integrity.
This dual action — immune modulation plus enhanced matrix production — produces measurable improvements such as lower pain scores, better range of motion, and stronger functional performance. Recognizing this synergy helps clinicians combine exosome injections with rehabilitation strategies that maximize structural and symptomatic recovery.
Which Tendon and Ligament Injuries Can Benefit from Exosome Therapy?
Exosome therapy can help a range of tendon and ligament problems where biological augmentation may support healing without immediate surgery. Common tendon indications include chronic tendinopathies and partial‑thickness rotator cuff tears, Achilles tendinopathy, and lateral epicondylitis (tennis elbow). Ligament use cases often include partial sprains and chronic instability where conservative care has failed but full reconstruction is not yet indicated. Choosing the right candidates depends on tear severity, chronicity, patient goals, and medical factors that affect healing potential.
Typical benefits from exosome treatment include better pain control, accelerated matrix remodeling, and functional recovery that supports progressive rehabilitation. When structural compromise is severe — for example, a full‑thickness rupture with gross instability — surgical evaluation remains essential. Exosomes work best for partial tears, chronic tendinopathy, and cases where biologic augmentation may prevent progression or speed recovery.
The table below links common conditions to their typical presentation and expected exosome‑related outcomes.
| Condition | Typical Cause / Presentation | Expected Exosome Benefit / Typical Outcomes |
|---|---|---|
| Achilles tendinopathy | Overuse or degenerative change of the mid‑portion or insertion | Less pain, improved tendon structure and load tolerance over weeks–months |
| Rotator cuff partial tears | Degenerative overload or acute strain | Lower local inflammation, enhanced tendon remodeling and shoulder function |
| Lateral epicondylitis (tennis elbow) | Repetitive wrist extension loading | Reduced pain, improved tendon healing, earlier return to activity |
| Patellar tendinopathy | Jumping or landing‑related overload | Better collagen alignment and less activity‑limiting pain |
| Ankle ligament sprain (partial) | Inversion injury with partial fiber disruption | Reduced swelling, improved stability when combined with rehab |
This overview clarifies typical use cases and realistic expectations. Patients with mixed pathology or prior surgeries usually benefit from a personalized diagnostic plan to determine candidacy and adjunctive strategies.
How Does Exosome Therapy Treat Common Tendon Injuries?
For tendinopathies such as Achilles or patellar degeneration, exosome injections aim to interrupt chronic low‑grade inflammation and stimulate collagen turnover, shifting the tissue from a degenerative matrix toward organized, load‑bearing collagen. In partial rotator cuff tears, targeted exosome delivery can lower inflammatory mediators and support healing at the tendon‑bone interface when paired with focused physiotherapy. For tennis elbow, exosomes address tendinosis by promoting fibroblast activity and matrix remodeling, often reducing pain and improving grip strength over weeks to months.
Timelines vary: many patients notice reduced pain and improved function within 4–12 weeks, with ongoing structural gains up to 6–12 months as collagen remodeling progresses. Repeat imaging or functional testing can track repair, and adjunct therapies — eccentric loading programs or manual therapy — help convert biological improvements into lasting performance gains.
What Ligament Conditions Respond Well to Exosome Injections?
Exosomes are most useful for ligament issues that preserve structural continuity: partial tears, chronic laxity from repetitive microtrauma, or delayed healing after sprains where non‑operative tissue restoration is realistic. Exosomes support ligament fibroblast proliferation and collagen realignment, which can improve stability and reduce pain when combined with a graded rehabilitation program. In some partial ACL or MCL injuries, exosome therapy is considered when the ligament is partially intact and the goal is to enhance intrinsic healing rather than replace it surgically.
Complete ruptures with mechanical instability usually require reconstruction, and clinicians watch for referral triggers such as recurrent giving‑way, high‑grade laxity, or failed functional progress. When used appropriately, exosomes can shorten recovery and improve tissue quality in ligament injuries suitable for biologic augmentation and conservative management.
Why Choose Exosome Therapy at Dr. Fred Bloem’s Holistic Regenerative Medicine Practice?
Exosome therapy gives the best results when it’s part of a comprehensive, patient‑centered plan that addresses both local and systemic healing factors. Dr. Fred Bloem’s practice emphasizes a holistic evaluation of metabolic, hormonal, nutritional, and functional contributors to tissue repair alongside targeted regenerative procedures. This integrative model focuses on root‑cause assessment, individualized protocols, and combining injections with evidence‑based rehabilitation and complementary regenerative services.
- Holistic assessment: A full evaluation uncovers systemic factors that may impede healing and allows optimization before biologic treatment.
- Personalized plans: Protocols are tailored to injury type, activity goals, and coexisting conditions to promote durable recovery.
- Regenerative expertise: The practice offers complementary options such as PRP and Prolozone, enabling blended strategies when clinically appropriate.
Selecting a clinic that pairs biologic treatments with nutrition, rehabilitation, and functional medicine improves results by addressing both local tissue deficits and overall healing capacity. This integrated approach also shapes how consultations and procedures are organized for a better patient experience and outcome.
What Are the Practical Benefits of Exosome Therapy for Joint Pain and Tissue Repair?
Exosome therapy is a minimally invasive, non‑surgical option for patients who want regenerative improvement without implants or long operative recovery. Clinically, exosomes can reduce inflammation, stimulate collagen remodeling, and improve function with relatively low downtime compared with surgery. For many people, the main advantages are faster symptom relief, improved tissue quality, and the ability to begin rehabilitation sooner while avoiding surgical risks.
Practically, exosomes appeal to patients who prefer a cell‑free biologic with a broad signaling payload that may be more consistent than autologous blood products. Combined with tailored physical therapy and metabolic optimization, exosome therapy can help patients return to sports, work, or daily life with stronger tissue and less recurrent pain.
How Does Dr. Bloem’s Personalized, Integrative Care Improve Outcomes?
Dr. Bloem’s practice conducts a thorough evaluation to identify modifiable barriers to healing — inflammation, hormonal imbalance, micronutrient gaps, and movement patterns — and addresses them with individualized plans. By pairing regenerative injections with targeted nutrition, hormonal optimization when needed, and progressive loading programs, patients follow a coordinated recovery path. Longer consultation times and clear patient education set realistic expectations and support adherence to rehab plans.
Combining regenerative procedures with supportive therapies reduces the chance of an isolated treatment failing and supports sustained functional gains. This integrated model aligns with growing evidence that biologic augmentation plus rehabilitation yields better results than either approach alone.
What to Expect During the Exosome Therapy Pathway for Tendon and Ligament Repair?

Most patients follow a clear pathway: an initial consultation and diagnostic assessment, a personalized treatment plan, an image‑guided injection, and a staged rehabilitation program with follow‑up checks. The consultation reviews history, a functional exam, and any imaging to confirm candidacy and optimize pre‑procedure factors. Injections are performed under sterile conditions with ultrasound guidance for precise delivery; the visit is brief and patients usually go home the same day with simple post‑procedure instructions.
The table below summarizes each step, what happens, and patient tips to support a smooth recovery.
| Step | What Happens | Patient Tips / Timeline |
|---|---|---|
| Consultation | Medical history, physical exam, imaging review, candidacy assessment | Bring prior imaging; expect a short optimization plan before injection |
| Procedure Visit | Ultrasound‑guided exosome injection under sterile technique | Quick procedure; mild soreness may occur; plan rest for 24–48 hours |
| Early Recovery | Controlled activity, icing, temporary activity modification | Avoid NSAIDs for the initial period if advised; begin gentle range‑of‑motion per instructions |
| Rehabilitation | Progressive loading and coordination with physical therapy | Gradual strengthening over 6–12 weeks to rebuild tendon load tolerance |
| Follow-up | Clinical reviews, functional assessments, possible repeat treatment | Expect symptom improvement at 4–12 weeks, with continued gains up to 6–12 months |
This stepwise plan sets clear expectations and supports shared decision‑making. Patients who optimize sleep, nutrition, and metabolic health before treatment typically have more consistent results.
How Is the Consultation and Diagnosis Performed?
A thorough consultation covers injury history, prior treatments, current limitations, and goals, followed by a focused musculoskeletal exam and review of imaging (ultrasound or MRI) when needed. Clinicians screen for factors that affect healing — metabolic health, systemic inflammation, medication use — and determine whether pre‑treatment optimization is recommended. Imaging helps plan the injection approach and identifies cases that need surgical referral instead of percutaneous biologic augmentation.
Pre‑procedure guidance often includes temporary adjustments to medications or supplements that affect inflammation or platelet function, optimizing blood sugar control if relevant, and planning a staged rehab program. Clear communication during the consult ensures realistic expectations and better adherence to recovery plans.
What Happens During the Injection and What Is the Recovery Timeline?
The injection is done in a sterile outpatient setting with ultrasound guidance to place the exosome preparation precisely at the injured tendon or ligament interface. Local anesthetic may be used for comfort. The entire visit generally takes less than 30 minutes including prep. Patients can expect some immediate soreness or a short inflammatory response that is usually managed with ice, activity modification, and brief pain control as directed.
Recovery varies by tissue and injury severity: many patients feel symptom relief within 4–12 weeks, with progressive functional improvements over 6–12 months as collagen remodeling matures. Rehabilitation focuses on graduated loading to restore tensile strength and function. Follow‑up visits track progress and determine whether adjunctive treatments or additional injections are needed.
How Does Exosome Therapy Compare with PRP and Stem Cell Treatments?
Exosomes differ from PRP and stem cell therapies in mechanism, composition, and practical considerations. Exosomes are cell‑free vesicles carrying concentrated signaling cargo; PRP is an autologous platelet‑rich concentrate from the patient’s blood; stem cell therapies introduce living cells intended to engraft or secrete reparative factors. These distinctions affect safety profiles, regulatory considerations, and clinical use cases.
The table below summarizes key attributes across these approaches.
| Approach | Key Characteristic | Typical Clinical Considerations |
|---|---|---|
| Exosome Therapy | Cell‑free extracellular vesicles carrying signaling molecules | Broad signaling profile; potential batch consistency; useful for non‑surgical augmentation |
| PRP (Platelet‑Rich Plasma) | Autologous platelets and growth factors derived from the patient’s blood | Lower cost; autologous safety; effective for many tendinopathies but potency varies by preparation |
| Stem Cell Therapy | Living cells intended to augment repair | Cell‑based mechanisms; more complex regulatory and safety considerations; may be appropriate in select scenarios |
This comparison helps patients and providers choose the approach that best fits clinical goals, available evidence, and safety preferences. Clear distinctions support informed, shared decision‑making.
What Advantages Do Exosomes Offer Compared with PRP?
Exosome products deliver a concentrated, cell‑free mix of signaling molecules — including microRNAs, proteins, and growth factors — that can be broader than the factors present in autologous PRP. Because exosomes are not living cells, they avoid some immunologic and regulatory issues tied to cell‑based therapies, and certain preparations may offer more consistent potency than variable PRP yields. For patients seeking a non‑autologous, standardized biologic signal, exosomes are an attractive option.
That said, PRP remains a valid, lower‑cost, autologous option with a solid evidence base for many tendinopathies. PRP may be preferred when patients want a treatment derived from their own blood and when cost or regulatory considerations favor autologous therapy.
How Do Exosomes Differ from Stem Cell Treatments?
Stem cell treatments introduce living cells that may persist and secrete reparative factors over time, while exosomes provide a concentrated paracrine signal without implanting donor cells. This difference changes the risk profile: exosomes reduce concerns about donor cell survival and cell‑related risks, whereas stem cell approaches may offer longer‑term biological activity but carry more complex safety and regulatory implications. Evidence is evolving for both strategies; stem cell interventions are typically reserved for select cases where cell‑based mechanisms are judged necessary.
Choosing between cell‑free and cell‑based options depends on injury severity, available data, regulatory context, and patient preference. In many tendon and ligament applications, exosomes and PRP provide effective, lower‑risk biologic augmentation compared with cell‑based approaches.
Frequently Asked Patient Questions About Exosome Therapy for Tendons and Ligaments
Patients commonly ask about expected benefits, timelines, side effects, and number of treatments. Current research and clinical experience show that many people experience meaningful symptom improvement within 4–12 weeks, with structural remodeling continuing for months. Response depends on age, injury chronicity, medical comorbidities, and adherence to rehabilitation. Typical side effects are mild and transient, such as injection‑site soreness or short inflammatory flares.
Below are concise answers to common questions.
- How long until I see results? Many patients report pain relief within 4–12 weeks, with continued improvement up to 6–12 months as tissue remodels.
- Is the procedure painful? Most patients tolerate the injection well with local anesthetic; short‑lived soreness afterward is common.
- How many treatments are needed? Protocols vary. Some patients improve after a single session; others may follow a planned series based on clinical response.
- Are there serious risks? Serious complications are uncommon. Proper screening and sterile technique minimize infection and other risks.
What Success Rates and Outcomes Can I Expect?
Reported success rates vary by study, condition, product, and adjunct rehab, but early data and clinical experience show meaningful symptom improvement for a substantial proportion of patients with tendinopathies and partial ligament injuries. Factors that improve odds of success include earlier intervention in degenerative processes, optimizing systemic health, and following a structured rehab plan. Outcome measures often include reduced pain scores, better functional tests, and improved load tolerance.
Because research continues to evolve, clinicians emphasize realistic expectations: biologic therapies support the body’s repair capacity but are not guaranteed cures. Careful patient selection and shared decision‑making remain central to achieving favorable outcomes.
What Risks or Side Effects Should I Know About?
Short‑term side effects typically include localized soreness, mild swelling, and transient inflammatory responses at the injection site; these are usually self‑limited and manageable with conservative measures. Rare risks may include infection or an unexpected inflammatory reaction — which is why sterile technique, careful patient screening, and experienced providers are essential. Pre‑procedure evaluation screens for contraindications and optimizes modifiable risk factors to reduce complications.
Regular follow‑up allows clinicians to monitor healing, address side effects quickly, and tailor rehabilitation. Overall, exosome therapy demonstrates a favorable safety profile when used within an appropriate clinical framework.
If you’re interested in regenerative options, Dr. Fred Bloem at Internal Healing and Wellness MD integrates exosome therapy with a full assessment and complementary services like PRP and Prolozone when appropriate. To schedule an initial consultation and personalized evaluation, contact the practice directly to discuss candidacy and next steps.
- Why choose a consultation? A consultation enables tailored planning and pre‑procedure optimization to improve outcomes.
- What should I bring? Bring your medical history and any prior imaging to help the clinician create an individualized plan.
- What sets this practice apart? The practice emphasizes a holistic assessment, personalized protocols, and integrated regenerative therapies.
These closing notes connect clinical information with practical next steps while keeping the focus educational and patient‑centered.
Frequently Asked Questions
What is the typical recovery timeline after exosome therapy?
Recovery varies by injury and individual factors. Generally, patients may notice pain and functional improvement within 4–12 weeks after the injection, with ongoing structural gains over 6–12 months as collagen remodels. Sticking to a structured rehab plan is important for the best outcome.
Are there any specific contraindications for exosome therapy?
While exosome therapy is generally well tolerated, certain contraindications exist. Active infection at the treatment site, known severe allergies to product components, or specific anticoagulant regimens may require further evaluation. A detailed consultation and medical history review identify potential risks and ensure the therapy is appropriate.
How does exosome therapy integrate with physical rehabilitation?
Exosome therapy is most effective when paired with a tailored rehabilitation program. After the injection, progressive loading and strengthening exercises help convert the biological gains into functional improvements and reduce re‑injury risk. Close coordination between the proceduralist and the rehab team optimizes recovery.
Can exosome therapy be used for acute injuries?
Exosomes are primarily used for chronic conditions and partial‑thickness injuries, but they can be helpful in some acute cases. If an acute injury involves significant tissue damage or instability, immediate surgical care may be required. A careful assessment determines whether exosome therapy can play a role in the early recovery phase.
What should I expect during the exosome injection procedure?
The procedure typically occurs in a sterile outpatient setting and is guided by ultrasound for accuracy. It usually lasts less than 30 minutes and often uses local anesthetic for comfort. Mild soreness or transient inflammation is common afterward, but most patients can resume light activity with recommended modifications.
How do I know if I am a good candidate for exosome therapy?
Candidacy is determined through a comprehensive clinical evaluation. The clinician will consider the type and severity of your injury, overall health, and past treatment responses. A review of your history and imaging helps determine whether exosome therapy fits your personalized treatment plan.
What are the long‑term benefits of exosome therapy?
Long‑term benefits can include lasting pain reduction, improved function, and better tissue quality. Many patients regain the ability to perform daily activities and return to sport or work with improved structural resilience. The goal is to support natural healing processes that lead to durable changes in affected tendons and ligaments.
Conclusion
Exosome therapy is a promising, non‑surgical option for many tendon and ligament injuries, harnessing the body’s natural repair signals to enhance recovery. By lowering inflammation and encouraging tissue regeneration, patients can expect improved symptom management and functional gains. A holistic, personalized approach maximizes the benefits of this evolving treatment. To learn whether exosome therapy is right for you, schedule a consultation with Dr. Fred Bloem at Internal Healing and Wellness MD.



