
Bioidentical vs. Synthetic Hormones: Clear Differences and What They Mean for Your Therapy
Your choice of hormone therapy affects symptom control, metabolic outcomes, and long‑term risk for people facing menopause, andropause, or other hormone imbalances. This article breaks down what we mean by “bioidentical” versus “synthetic” hormones at the molecular level, how each interacts with hormone receptors, and why those differences matter for symptom relief, monitoring, and safety. You’ll find clear explanations of biochemical definitions, common formulations and delivery methods, and the clinical trade‑offs between bioidentical hormone replacement therapy (BHRT) and conventional HRT. We also review typical indications, summarize the evidence, and answer the questions patients ask most often so you can make informed choices.
Sections include: how bioidentical hormones are defined and work; the chemical distinctions of synthetic hormones; who may benefit from BHRT and how individualized testing guides care; a direct comparison of BHRT and traditional HRT; and concise FAQs about safety and limitations. Throughout, terms like bioidentical hormone replacement therapy, BHRT, synthetic hormones, HRT vs BHRT, and personalized hormone therapy appear to keep concepts clear and clinically useful.
What Are Bioidentical Hormones and How Do They Work?
Bioidentical hormones are compounds that share the same chemical structure as the hormones your body makes, so they bind the same receptors and trigger familiar physiological responses. Molecular identity affects receptor affinity and downstream signaling, which is why bioidentical estradiol, progesterone, or testosterone tend to mimic natural hormone‑receptor interactions and metabolic pathways. That likeness supports symptom relief when dosing is tailored to an individual’s serum levels or metabolite patterns. Clinicians select formulations and delivery routes to match each patient’s needs, while monitoring metabolic and cardiovascular markers. Knowing the pharmacology behind bioidentical hormones explains why personalization and testing are central to BHRT and why results can differ from standardized synthetic regimens.
What Defines Bioidentical Hormones and Their Natural Sources?
Bioidentical hormones are defined by molecular equivalence to human hormones and are typically derived from plant precursors before being converted into hormones identical to those in the body. Common sources include diosgenin from wild yam or soy sterols that are synthesized under controlled conditions into estradiol, progesterone, or testosterone molecules that match endogenous structures. Compounded bioidentical products allow clinicians to tailor dose and delivery (creams, pellets, injections, oral formulations) to a patient’s needs, but consistent potency requires rigorous pharmacy standards and clinician oversight. That molecular match influences receptor binding, metabolism, and physiological effects compared with structurally altered synthetic molecules.
What Are the Benefits of Bioidentical Hormone Therapy?

Bioidentical hormone replacement therapy aims to reduce common symptoms of hormone imbalance while supporting functional health through individualized dosing and monitoring. In clinical practice and integrative medicine, patients frequently report improvements in hot flashes and night sweats, sleep quality, libido, mood stability, and preservation of lean body mass and skin health when hormones are restored to appropriate levels. Personalized protocols that use serum panels or advanced metabolite testing allow clinicians to adjust dose and delivery to optimize symptom control and limit side effects. Many patients notice gradual improvements within weeks, with fuller benefit over months, and ongoing monitoring guides safe, effective adjustments.
- Targeted symptomatic relief often includes fewer hot flashes, improved sexual function, and better energy and sleep.
- Functional gains can include sharper cognition, steadier mood, and improved body composition when estrogen and testosterone are balanced.
- Quality‑of‑life results depend on individualized dosing, close follow‑up, and integration with lifestyle measures to sustain benefit.
These outcomes are most reliable when BHRT is part of a structured care plan that includes follow‑up testing and patient education to measure response and safety.
How Do Synthetic Hormones Differ from Bioidentical Hormones?
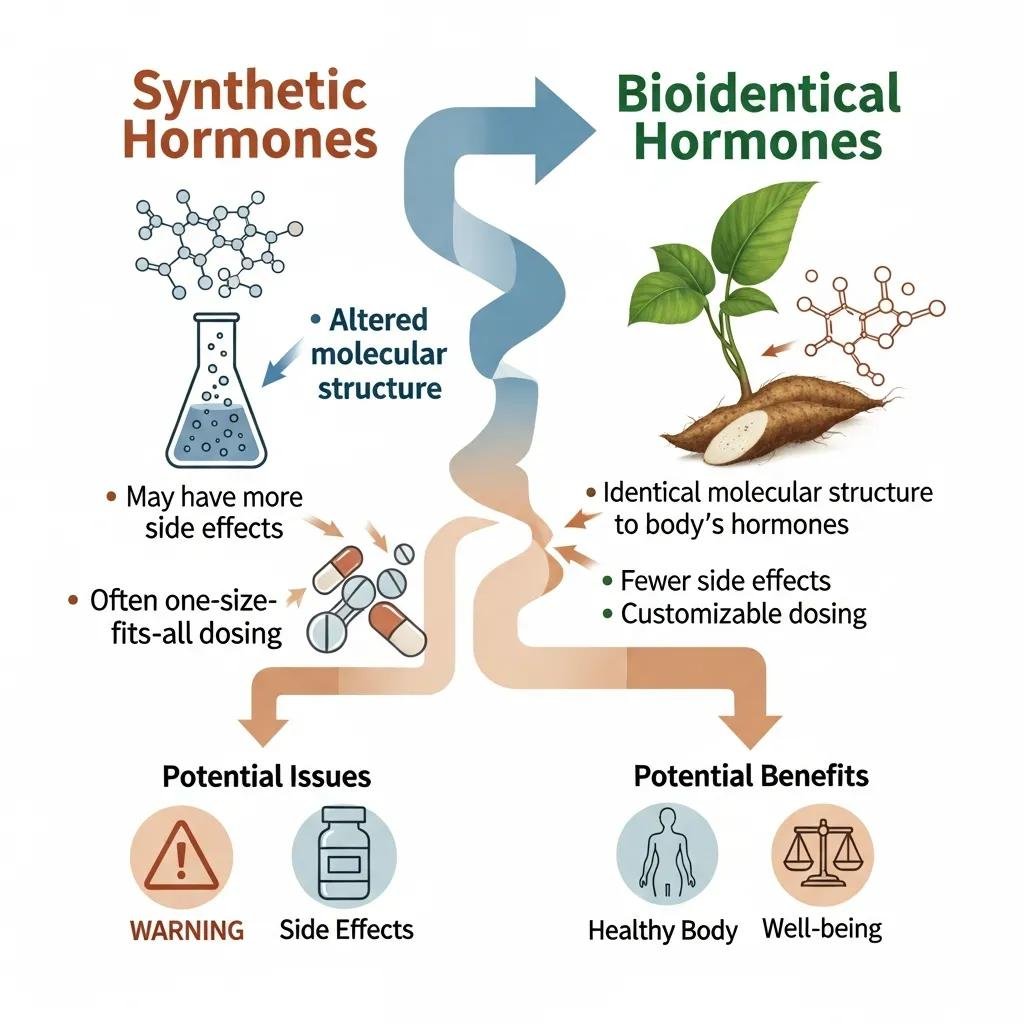
Synthetic hormones are chemically modified molecules or non‑human‑derived estrogens and progestogens formulated for predictable pharmacokinetics and standardized dosing. Structural differences can change how they interact with receptors and how they’re metabolized. Examples include conjugated equine estrogens and certain progestins that contain substitutions or side chains not found in human hormones; those changes affect tissue selectivity, half‑life, and downstream risk profiles. Conventional HRT products are typically manufactured at fixed doses and approved for broad indications, offering standardized options for symptom control but with different monitoring and safety considerations than individualized BHRT. Clinicians weigh these distinctions when recommending therapy for menopause symptoms, contraception adjuncts, or other endocrine needs.
What Is the Chemical Composition of Synthetic Hormones?
Synthetic hormone compounds often include structural changes—alkylations, oxygenation shifts, or sulfate conjugations—that improve oral bioavailability or extend duration of action but do not replicate the exact geometry of human hormones. For instance, conjugated non‑human estrogens are mixtures of estrogenic molecules with sulfate conjugates derived from animal sources, while many progestins are engineered for oral stability. Those modifications influence receptor subtype activation and metabolite formation and can have meaningful clinical implications for tissue effects and side‑effect patterns. That’s why clinicians consider both efficacy and individual risk when prescribing traditional HRT.
Diverse synthetic compounds are used in practice, and their differing structures explain variations in therapeutic window, monitoring needs, and adverse‑effect profiles.
| Formulation Type | Chemical Characteristic | Clinical Implication |
|---|---|---|
| Conjugated estrogens (non-human) | Mixture of linked sulfate estrogens | Broad estrogenic activity, variable metabolites |
| Synthetic progestins | Structural side-chain modifications | Altered receptor selectivity and metabolic effects |
| Modified androgens | Alkylation or esterification | Prolonged action, different hepatic effects |
What Are the Risks and Side Effects of Synthetic Hormone Replacement?
Conventional synthetic HRT carries known adverse‑event patterns that clinicians monitor, including thromboembolic risk, variable effects on breast and endometrial tissue, and cardiovascular considerations tied to baseline patient risk. Population studies and guideline bodies have identified risk signals with some formulations and dosing strategies, so individualized risk assessment is essential before starting therapy. Mitigation includes careful patient selection, the lowest effective dose for symptom control, routine surveillance, and choosing alternative formulations for those with risk factors. Shared decision‑making with a clinician who monitors metabolic and hematologic markers helps balance benefits and harms for each patient.
- Monitoring typically focuses on blood pressure, lipid profile, liver function, and symptom‑driven assessments.
- Rare but serious risks—such as venous thromboembolism—are associated with particular products and patient risk profiles.
- Risk reduction strategies include personalized dosing, alternative delivery routes, and scheduled follow‑up testing.
Recognizing these risks and the ways to monitor and reduce them helps patients and clinicians choose the most appropriate therapy.
Who Can Benefit from Bioidentical Hormone Replacement Therapy?
BHRT can be appropriate for adults with symptoms from menopause, perimenopause, andropause, or other hormone imbalances where restoring physiological hormone levels improves quality of life. Candidate selection combines clinical symptoms, laboratory testing, and review of comorbidities. Common goals include reducing vasomotor symptoms, restoring sexual function, improving energy and sleep, and supporting metabolic health. Individualized testing—such as serum hormone panels or detailed metabolite profiles—helps clinicians tailor hormone type, dose, and delivery while planning monitoring intervals. Timelines for symptom improvement vary: some vasomotor relief can appear within weeks, while broader quality‑of‑life gains often take months.
Which Conditions Are Treated with BHRT?
BHRT is used for a range of hormone‑related conditions in men and women where restoring physiological hormone levels is clinically indicated. Typical uses include menopausal vasomotor symptoms, perimenopausal irregularities, symptomatic low testosterone in men (andropause), libido concerns, and as an adjunct in certain functional medicine approaches for fatigue or mood disturbance. Treatment strategy varies by condition: estrogen‑focused therapy for vasomotor symptoms, progesterone for endometrial protection and mood support, and testosterone when clinically indicated for low desire or energy issues.
- Menopause: Hot flashes, night sweats, vaginal dryness, disrupted sleep.
- Andropause: Low libido, reduced muscle mass, fatigue, cognitive slowing.
- Adjunctive: Fatigue syndromes and select functional medicine plans where hormones are one part of a broader strategy.
Careful candidate selection and testing ensure BHRT targets the symptoms most likely to improve, with measurable goals and planned follow‑up.
How Does Dr. Fred Bloem’s Holistic Approach Enhance BHRT Outcomes?
Dr. Fred Bloem combines a root‑cause evaluation with individualized BHRT protocols, longer patient visits, and thorough patient education to support adherence and outcomes. The clinic emphasizes comprehensive testing and personalized dosing plans, and when appropriate integrates BHRT with anti‑aging and regenerative therapies to support wider functional health goals. This patient‑centered model—built on individualized assessment and ongoing partnership—helps set realistic timelines, clarify objectives, and adjust therapy based on objective monitoring and patient experience. Patients in Kensington, MD seeking tailored hormone care will find longer consultations and coordinated wellness services designed to support sustainable improvements.
What Are the Main Differences Between BHRT and Traditional HRT?
BHRT and traditional HRT mainly differ in molecular identity, degree of customization, regulatory status, and monitoring approach—factors that shape patient experience and clinical decisions. BHRT emphasizes molecular equivalence to endogenous hormones and may use compounded or standardized bioidentical products tailored to the individual, while traditional HRT relies on approved synthetic or non‑human‑derived products with fixed doses. Customization allows BHRT to adjust delivery methods (pellets, creams, injections, oral) and dosing based on metabolite profiles; traditional HRT generally follows standardized regimens supported by large trials. These differences influence monitoring, counseling on risks, and therapy choice according to patient preferences and risk profiles.
| Attribute | BHRT (Bioidentical) | Traditional HRT (Synthetic/Conventional) |
|---|---|---|
| Molecular identity | Matches endogenous hormones | Modified or non-human estrogens/progestogens |
| Customization | Individualized dosing, compounding options | Standardized doses and formulations |
| FDA/regulatory status | Mix of compounded and regulated products | Widely FDA-approved products with large trials |
| Monitoring | Frequent individualized testing | Routine guideline-driven monitoring |
| Typical risk profile | Dependent on formulation and patient | Well-characterized population-level risks |
How Do BHRT and HRT Compare in Safety and Efficacy?
Evidence comparing BHRT and traditional HRT is still developing. Both approaches can relieve common symptoms, but direct head‑to‑head randomized data are limited for many compounded BHRT regimens. Traditional HRT has clearer, large‑trial evidence defining benefits and risks, whereas BHRT offers theoretical advantages from molecular matching and individualized dosing but relies on careful pharmacy standards and monitoring. Clinician choice often reflects patient priorities, baseline risk, and willingness to undergo individualized titration versus using standardized regimens. Regardless of the product, safety depends on proper selection, the lowest effective dose, and regular reassessment.
- Key decision factors include age, cardiovascular and cancer history, symptom severity, and preference for customization.
- Monitoring principles are similar, though individualized BHRT may require more frequent checks to confirm potency and metabolite balance.
- Shared decision‑making and informed consent are essential given evidence gaps and patient variability.
What Does the Hormone Therapy Comparison Chart Reveal?
The comparison chart highlights the most practical differences: molecular match, degree of personalization, and the type of evidence supporting each approach. Use the chart to compare molecular identity, formulation options, monitoring requirements, and documented outcomes, and interpret it alongside your personal health profile and clinician guidance. The main takeaways: customization can improve symptom targeting, standardized products offer clearer population‑level safety data, and both pathways require follow‑up to maximize benefit and reduce risk.
- Chart tip: focus on attributes that matter most to you—safety data if you’re high‑risk, customization if prior therapy failed.
- Practical next step: ask your clinician how monitoring will be handled and what objective measures indicate success.
- Clinical takeaway: match scientific evidence, molecular considerations, and patient priorities when choosing therapy.
After weighing these differences, many patients choose a provider‑led, individualized plan that emphasizes education and follow‑up—an approach available from integrative practices offering BHRT alongside complementary therapies.
What Are Common Questions About Bioidentical and Synthetic Hormones?
Patients often want to know whether bioidentical hormones are safer, what downsides exist, and how to decide between BHRT and traditional HRT. The following concise, evidence‑aware answers address the most common concerns: safety nuances, regulatory variability, monitoring needs, and situations where one approach may be preferable. These responses assume shared decision‑making with a qualified clinician who can interpret tests and risk factors in light of current evidence and guidelines.
Are Bioidentical Hormones Safer Than Synthetic Hormones?
There’s no blanket answer—safety depends on the specific molecule, dose, delivery route, and individual risk profile. Some synthetic formulations have population‑level risk signals for thromboembolism or cardiovascular outcomes, while bioidentical hormones offer theoretical advantages from molecular matching but lack similarly large randomized trial data for many compounded preparations. Clinician oversight, appropriate testing, and ongoing monitoring are critical to minimize risk with either approach. Ultimately, an individualized assessment determines which option best balances symptom relief and safety for a given patient.
- Bottom line: molecular identity influences receptor behavior but does not by itself determine safety.
- Clinical steps: assess baseline risk, use the lowest effective dose, and monitor relevant biomarkers.
- Talk with your clinician about evidence limitations and the planned monitoring strategy.
What Are the Disadvantages of Bioidentical Hormones?
Potential disadvantages of bioidentical hormones include variability in compounded product quality, differences in regulatory oversight, and fewer large randomized trials for some formulations. Compounded BHRT can vary between pharmacies unless sourced from certified compounding facilities with strict quality control, which makes pharmacy selection important. Individualized regimens may require more frequent monitoring and dose adjustments, increasing follow‑up burden compared with some standardized HRT options. In situations where large‑trial data support a particular synthetic product for a high‑risk patient, conventional HRT may remain the preferred, evidence‑based choice.
- Variability: compounding can introduce potency and consistency differences.
- Evidence gap: fewer large randomized trials for many compounded BHRT products.
- Monitoring burden: personalized plans may need more frequent testing and visits.
These trade‑offs underscore the importance of clinician guidance and choosing reputable compounding pharmacies or regulated bioidentical products.
For patients seeking individualized hormone care with integrated support, Internal Healing and Wellness MD in Kensington, MD, offers a patient‑centered model with longer visits, comprehensive testing, and tailored protocols. The practice provides holistic and integrative medicine, BHRT, anti‑aging strategies, regenerative joint therapies, and IV therapies, all delivered with an emphasis on patient education and partnership to improve outcomes.
If you’re ready to explore personalized hormone strategies, scheduling an initial consultation with Dr. Fred Bloem offers a root‑cause evaluation, comprehensive testing, and a tailored treatment plan aligned with your goals. The clinic prioritizes shared decision‑making, extended appointment time for education, and appropriate integration of BHRT with complementary therapies. If you have ongoing symptoms of menopause, andropause, or hormone imbalance, a focused evaluation can clarify whether BHRT, traditional HRT, or a combined approach best fits your profile and preferences.
This information is intended to empower patients to ask specific questions about molecular identity, monitoring plans, and follow‑up schedules when discussing hormone therapy options with their clinician.
Frequently Asked Questions
What is the role of hormone testing in determining the need for BHRT?
Hormone testing is key to identifying imbalances that may warrant BHRT. Clinicians commonly use serum hormone panels or detailed metabolite profiles to assess estrogen, progesterone, and testosterone levels. These results inform personalized dosing and delivery choices. Regular follow‑up testing ensures levels remain in the target range, helping optimize outcomes and reduce side effects.
How long does it take to see results from BHRT?
Response time varies. Many patients notice improvements in hot flashes, mood, and energy within a few weeks of starting therapy. More comprehensive benefits—such as improved sleep, body composition, and overall quality of life—often take several months. Ongoing follow‑up lets clinicians fine‑tune dosing to maximize benefit.
Can men benefit from bioidentical hormone therapy?
Yes. Men experiencing symptomatic low testosterone—fatigue, reduced libido, loss of muscle mass, or cognitive changes—may benefit from BHRT. As with women, individualized testing and careful monitoring are essential to tailor treatment safely and effectively to each man’s needs.
What lifestyle changes can enhance the effectiveness of BHRT?
Healthy habits complement BHRT. Regular exercise, a balanced whole‑food diet, adequate sleep, and stress management support hormone balance. Avoiding tobacco and limiting alcohol also helps. Work with your provider to create a wellness plan that supports your hormone therapy and overall goals.
Are there specific dietary recommendations for patients undergoing BHRT?
There are no strict dietary rules, but a nutrient‑rich diet supports hormonal health. Emphasize fruits, vegetables, lean proteins, healthy fats, and whole grains. Foods with phytoestrogens—like flaxseed or soy—may be beneficial for some people. Stay hydrated, limit processed foods and excess sugar, and consider consulting a nutritionist for personalized guidance.
What should patients expect during their initial consultation for BHRT?
Expect a comprehensive visit: detailed medical history, symptom review, and lifestyle assessment. Your clinician will likely order hormone testing to identify imbalances and discuss potential benefits, risks, and treatment goals. The appointment focuses on creating a personalized plan that reflects your health priorities and preferences.
Conclusion
Choosing between bioidentical and synthetic hormones matters because each option offers different advantages depending on your goals and risk profile. Understanding molecular differences, customization options, and monitoring requirements helps you make an informed decision with your clinician. For individualized guidance and a thorough evaluation, consider scheduling a consultation with a qualified provider. Taking that step can move you toward better symptom control and improved quality of life.



