
Achieving Estrogen & Progesterone Balance with Bioidentical Hormone Replacement Therapy for Women: A Clear, Practical Guide to Symptoms, Benefits, and Whole‑Person Care
Balanced estrogen and progesterone are central to mood stability, restorative sleep, reproductive health, bone strength, and overall well‑being for women. When one hormone outweighs the other—whether estrogen dominance or low progesterone—symptoms like hot flashes, poor sleep, weight shifts, mood changes, and irregular cycles can disrupt daily life. This guide explains how bioidentical hormone replacement therapy (BHRT) works to reestablish hormonal balance, outlines likely benefits and safety considerations, and reviews complementary, functional medicine strategies that support lasting results. You’ll learn how to spot common imbalance signs, what tests clinicians use, how bioidentical hormones act, and how lifestyle, detox, and integrative therapies fit alongside individualized BHRT and monitoring. Keywords such as estrogen balance, progesterone therapy, BHRT for women, and hormone testing for women are woven through to connect clinical ideas to practical next steps.
Restoring Estrogen & Progesterone Balance with BHRT

When estrogen and progesterone are out of proportion, one hormone’s excess or one’s insufficiency creates a recognizable cluster of physical and emotional signs. These hormones influence multiple systems—reproductive health, sleep, mood, metabolism, and bone—so early recognition helps prioritize testing and targeted care. If symptoms persist or worsen, a clinical evaluation can determine whether BHRT or integrative therapies could restore balance and improve daily functioning.
Common symptoms of estrogen and progesterone imbalance include:
- Hot flashes and night sweats: Sudden waves of heat and sweating that interrupt sleep and comfort.
- Mood swings and anxiety: Increased irritability, low mood, or heightened anxiety tied to hormonal shifts.
- Irregular periods and fertility changes: Variable cycle length, heavy bleeding, or trouble conceiving.
- Sleep disturbances and insomnia: Difficulty falling or staying asleep, often linked to inadequate progesterone.
- Low libido and vaginal dryness: Decreased sexual desire and mucosal thinning related to hormone imbalance.
- Fatigue and brain fog: Persistent low energy and concentration difficulties that interfere with daily tasks.
- Weight changes and bloating: Central weight gain and fluid retention commonly associated with estrogen excess.
- Breast tenderness and fibrocystic changes: Cyclical breast pain and fluctuations in breast density.
These patterns help clinicians distinguish estrogen dominance from progesterone deficiency and guide which hormone tests will be most informative. Spotting the right symptom clusters makes it easier to design targeted testing and treatment plans.
How Does Estrogen Dominance Affect Women's Health?
Estrogen dominance describes a state where estrogen activity outpaces progesterone, whether from the body’s own production, external exposures, or slowed metabolic clearance. Excess estrogen can increase tissue proliferation in estrogen‑sensitive areas, shift neurotransmitter balance, and promote water retention—explaining heavier periods, breast tenderness, fluid buildup, and mood swings. If left unaddressed, this pattern can worsen PMS, contribute to fibrocystic changes, and create low‑grade inflammation that undermines quality of life.
Clinically, we look for timing clues—worse symptoms in the luteal phase, persistent breast sensitivity, or unexplained weight gain—that point toward relative progesterone insufficiency or impaired estrogen detoxification. A thorough assessment includes liver and gut function, thyroid status, and environmental exposures to build a comprehensive plan. Addressing estrogen dominance usually combines hormone rebalancing with metabolic and lifestyle supports for lasting improvement.
What Are the Signs of Low Progesterone and Its Impact?
Low progesterone typically shows up as sleep problems, increased anxiety, spotting mid‑cycle or a short luteal phase, and difficulty sustaining early pregnancy. Progesterone supports calming GABA pathways and stabilizes the menstrual cycle, so deficiency often presents as insomnia, restlessness, and emotional reactivity. Those pursuing pregnancy may notice luteal phase defects or early pregnancy losses related to insufficient progesterone support.
Timing matters for testing: luteal‑phase blood draws or cycle‑timed saliva/urine panels give actionable progesterone data relative to your cycle day. Treatment focuses on restoring adequate luteal progesterone to normalize cycles, improve sleep and mood, and support fertility when relevant. Recognizing low progesterone informs choices—micronized progesterone, transdermal formulations, or combined BHRT—and highlights the importance of individualized testing and follow‑up.
How Does Bioidentical Hormone Replacement Therapy Work to Restore Hormone Balance?
Bioidentical hormone replacement therapy (BHRT) uses hormones that match the molecular structure of your body’s own estrogen and progesterone so they interact naturally with hormone receptors and restore physiologic signaling. Plant‑derived precursors are converted into estradiol or micronized progesterone that support gene expression, neurotransmitter balance, bone metabolism, and menstrual regulation. Clinically, BHRT follows a testing‑to‑treatment workflow: targeted hormone testing guides individualized dosing and route selection, and ongoing monitoring refines safety and effectiveness.
Brief explanation of how bioidentical hormones act:
| Hormone | Attribute | Mechanism |
|---|---|---|
| Estradiol (E2) | Primary bioidentical estrogen | Binds estrogen receptors to support bone density, cardiovascular and vascular health, and vaginal mucosal integrity |
| Progesterone (micronized) | Natural progestogen | Modulates GABA pathways to stabilize mood and sleep; protects the endometrium and supports the luteal phase |
| Delivery methods | Pellets, creams, oral, transdermal | Affect absorption and steady‑state levels, so route choice changes pharmacokinetics and clinical effect |
This overview shows how matching hormone structure to native molecules produces targeted physiologic effects and sets the stage for the individualized BHRT pathway clinicians use to optimize care.
What Are Bioidentical Hormones and How Are They Different from Traditional HRT?
Bioidentical hormones share the exact chemical structure of human hormones and are generally made from plant‑derived precursors. Traditional HRT can include synthetic analogs or conjugated equine estrogens with different molecular shapes. Because bioidentical hormones more closely mimic endogenous hormones, they tend to produce physiologic responses and allow flexible dosing strategies. Research supports symptom relief from bioidentical estradiol and micronized progesterone, but safety considerations—common to all systemic hormone therapies—remain important and are actively monitored by clinicians.
Patients and providers should consider formulation, route, and a monitoring plan alongside clinical goals and medical history. Clear testing and thoughtful follow‑up help tailor whether transdermal estradiol with cyclic micronized progesterone or another regimen best fits individual needs.
What Is the Step-by-Step BHRT Process at Dr. Bloem's Clinic?
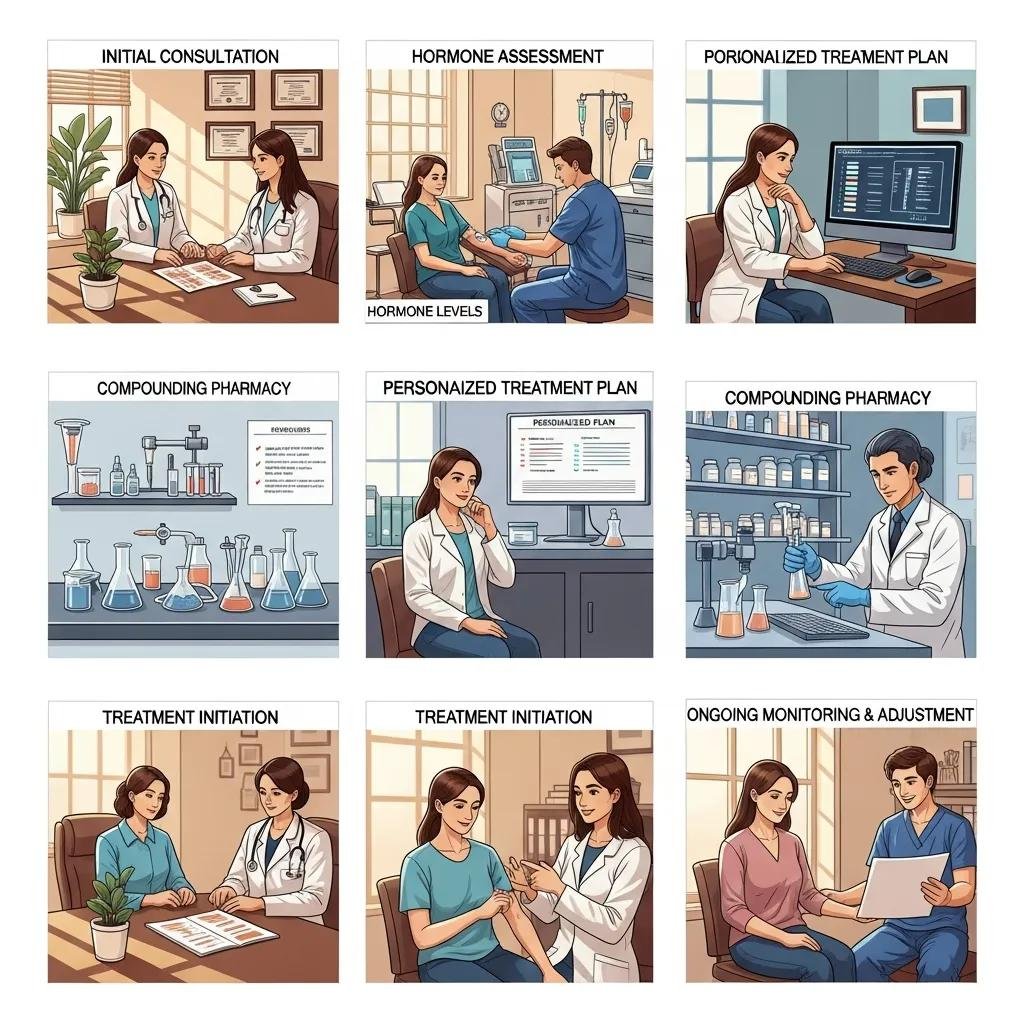
At a functional BHRT practice the care pathway typically starts with a focused consultation to review symptoms, medical history, and treatment goals. We then order targeted hormone testing—blood, saliva, or urine panels timed to your cycle when appropriate—and build an individualized plan that specifies hormone type, dose, and delivery route. Options may include transdermal estradiol, micronized progesterone, or longer‑acting pellet approaches. After starting therapy, scheduled follow‑ups and repeat testing assess symptom response and safety markers so we can fine‑tune dose and integrate supportive treatments.
Dr. Fred Bloem and the Internal Healing and Wellness MD team emphasize personalized protocols that pair BHRT with root‑cause assessment and adjunctive services; patients progress through consult → test → customize → administer → monitor → adjust. This structured approach promotes symptom relief while maintaining clinical oversight and individualized adjustments for safer, more durable outcomes.
What Are the Benefits and Risks of BHRT for Women's Hormone Health?
When chosen carefully, BHRT can significantly reduce hot flashes, improve sleep, stabilize mood, restore libido, and support bone and vaginal health by reestablishing more physiologic hormone signaling. Benefits must be balanced against risks that depend on hormone type, dose, route, and personal medical history. Safety strategies include baseline screening, selecting appropriate routes (for example, transdermal estradiol to lower thrombotic risk), and regular symptom and lab monitoring. Understanding this benefit‑risk balance helps you and your clinician make informed, personalized decisions.
| Hormone / Method | Potential Benefits | Considerations / Risks |
|---|---|---|
| Bioidentical estradiol (transdermal) | Reduces vasomotor symptoms, supports vaginal health, may protect bone | Less first‑pass liver effect than oral estrogens; requires screening for breast and cardiovascular risk |
| Micronized progesterone (oral or topical) | Helps sleep and mood, protects the endometrium when combined with estrogen | Can cause sedation in some people; timing and dosing matter for luteal support |
| BHRT pellets | Steady, long‑acting hormone levels and improved adherence | Minor office procedure required; dosing and monitoring must be individualized |
| Creams/topicals | Targeted relief for vaginal dryness and flexible dosing | Absorption varies; systemic levels may be inconsistent |
This table aligns benefits with delivery choices and highlights key safety conversations. Many patients find carefully supervised BHRT improves quality of life when combined with monitoring and metabolic support.
For patients seeking personalized BHRT within a functional medicine framework, Dr. Fred Bloem / Internal Healing and Wellness MD offers tailored hormone protocols alongside complementary services such as regenerative joint therapies and intravenous nutrient support. The practice emphasizes education and shared decision‑making so you understand options, monitoring, and how treatment fits your long‑term wellness goals. To discuss individualized BHRT and whether it fits your plan, contact the clinic to schedule a consultation.
How Does BHRT Improve Menopause and Perimenopause Symptoms?
BHRT often reduces vasomotor symptoms—hot flashes and night sweats—within weeks, improves sleep and mood over several weeks to months, and restores sexual comfort and vaginal health with ongoing therapy. Estradiol helps stabilize hypothalamic thermoregulation, while progesterone supports GABAergic tone that promotes restful sleep and emotional steadiness. Bone and urogenital improvements typically become measurable over months, and many patients notice gradual gains in energy and mental clarity as hormone balance is optimized.
Realistic expectations and scheduled follow‑up are important: some symptoms respond quickly, while bone and metabolic benefits accrue more slowly. Regular monitoring allows dose refinement and timely management of any side effects.
What Are the Potential Risks and Safety Measures in BHRT?
Adverse effects depend on dose, route, and individual risk factors and can include thrombotic risk with certain estrogen formulations, changes in breast density, fluid retention, or mood shifts. Contraindications and a patient’s medical profile guide safe prescribing. Safety measures include baseline cardiovascular and breast screening when indicated, choosing lower‑risk routes (for example, transdermal estradiol rather than high‑dose oral estrogen in at‑risk patients), and routine symptom review and laboratory testing.
Clinicians mitigate risk by selecting the appropriate hormone type and route, using progesterone for endometrial protection when needed, and adjusting doses based on symptoms and objective findings. Promptly reporting new symptoms and keeping scheduled follow‑ups help detect and address issues early.
| Hormone Type | Attribute | Value |
|---|---|---|
| Estradiol (transdermal) | Benefit | Effective for hot flashes with lower hepatic impact |
| Micronized progesterone | Benefit | Neurostabilizing and endometrial protective |
| Pellets | Attribute | Sustained delivery; requires office insertion and follow‑up |
This concise comparison helps clinicians and patients weigh mechanistic attributes against clinical outcomes to make evidence‑informed, safer choices.
How Can Holistic and Functional Medicine Support Estrogen and Progesterone Balance?
Holistic and functional approaches strengthen BHRT by improving metabolism, detoxification, nutrition, and lifestyle factors that shape hormone production, receptor sensitivity, and elimination. Interventions address liver phase I/II detox pathways, the gut microbiome (which influences estrogen recirculation), body composition, sleep, and stress—each important to estrogen‑progesterone balance. When combined with BHRT, these strategies reduce symptom recurrence and treat underlying contributors rather than only replacing hormones.
| Intervention | Intervention Type | Expected Effect |
|---|---|---|
| Dietary modification (fiber, cruciferous vegetables) | Nutrition | Supports estrogen metabolism and healthy body weight |
| Regular aerobic and resistance exercise | Lifestyle | Improves insulin sensitivity and favorably alters sex hormone binding |
| Stress reduction (mindfulness, CBT) | Behavioral | Reduces cortisol burden that can disrupt reproductive hormones |
| IV nutrient therapy / detox support | Integrative therapy | Repletes cofactors and supports metabolic detox pathways |
These interventions enhance BHRT by improving hormone clearance, lowering systemic inflammation, and building metabolic resilience—creating a stronger foundation for lasting balance.
What Natural Strategies Enhance Hormone Balance Alongside BHRT?
Simple, evidence‑based lifestyle, dietary, and targeted supplement strategies can support hormone metabolism and receptor responsiveness when coordinated with clinical BHRT. A fiber‑rich diet with cruciferous vegetables helps estrogen conjugation and elimination; resistance training preserves lean mass and improves insulin sensitivity, reducing peripheral aromatization that raises estrogen levels. Good sleep hygiene and stress management protect cortisol rhythms that otherwise disrupt reproductive hormones.
Practical strategies include:
- Dietary focus: Emphasize fiber and cruciferous vegetables to support estrogen clearance and gut health.
- Regular exercise: Combine aerobic activity with resistance training to improve metabolic health and hormone balance.
- Sleep optimization: Prioritize consistent, restorative sleep to support progesterone’s restorative effects.
These low‑risk, clinically sensible measures complement BHRT and should be tailored with your clinician’s guidance.
How Do Integrative Therapies Like Detoxification and IV Treatments Complement BHRT?
Integrative approaches—targeted detox protocols and IV nutrient infusions—aim to restore cofactors needed for hormone synthesis and clearance, lower inflammatory burden, and correct micronutrient gaps that impair endocrine function. Typical IV goals include repleting magnesium, B vitamins, and antioxidants to support methylation and liver detox pathways. Detox plans focus on safe, clinician‑supervised strategies to enhance biotransformation and reduce exposure to environmental estrogenic compounds.
These therapies are adjuncts, not replacements for BHRT; evidence varies by modality, so discuss potential benefits, limitations, and risks with your clinician before starting integrative treatments.
| Supportive Approach | Intervention | Expected Effect |
|---|---|---|
| Nutrition and gut health | Fiber, probiotics | Improves estrogen excretion and reduces reabsorption |
| Targeted supplementation | Magnesium, B‑vitamins | Supports sleep, mood, and methylation pathways |
| IV nutrient therapy | Clinician‑directed infusions | Rapid repletion of deficient cofactors to support metabolic function |
This comparison clarifies how integrative modalities can support hormone therapies and underscores the need for individualized planning and monitoring.
Why Choose Dr. Fred Bloem's Personalized Approach to Hormone Therapy?
Dr. Fred Bloem and the Internal Healing and Wellness MD team center care on individualized protocols that combine BHRT with root‑cause functional assessment, extended visits for patient education, and a suite of complementary services designed to optimize hormone balance and overall health. The practice emphasizes thorough testing, tailored dosing, and integration of supportive therapies—such as regenerative joint care and IV nutrient support—so hormone optimization becomes part of a broader restoration plan. Personalization improves safety by matching route and dose to your physiology and risk profile while supporting adherence and measurable outcomes.
How Does Personalized Treatment Optimize Hormone Balance and Wellness?
Individualization matters because hormone needs depend on age, menopausal stage, metabolic health, and symptom goals. Tailoring hormone type, dose, and route improves effectiveness and reduces unwanted effects. Personalized care uses baseline and follow‑up testing to align progesterone timing, estradiol dose, and delivery route with physiologic targets, and it pairs hormone therapy with lifestyle changes to address contributors like insulin resistance or impaired detoxification. Close monitoring allows gradual adjustments rather than abrupt changes, improving tolerability and lasting symptom control.
This patient‑centered approach supports better outcomes—improved sleep, more stable mood, and preserved bone health—and explains why a functional medicine framework often produces more durable benefits than a one‑size‑fits‑all prescription.
What Success Stories and Testimonials Demonstrate BHRT Effectiveness?
Patients frequently report clearer energy, better sleep, improved mood, and restored sexual function after appropriate BHRT combined with lifestyle optimization. The clinic documents these outcomes through anonymized case summaries and patient feedback. While individual responses vary, common themes include fewer vasomotor symptoms, more regular cycles, and better day‑to‑day functioning when hormone therapy is paired with metabolic and detox supports. The practice collects structured outcome data and patient narratives to inform continuous quality improvement and to set realistic expectations.
Prospective patients are invited to review anonymized case formats and patient stories available through the clinic to learn typical trajectories and expected monitoring timelines.
What Should You Know Before Booking a Consultation for BHRT?
Preparing for a BHRT consultation speeds diagnosis and personalizes testing. Gather a symptom diary, relevant medical history, prior lab results, and a list of current medications and supplements—this information helps the clinician design a targeted testing plan. Expect your initial visit to include a detailed history, a discussion of testing options, and an explanation of potential therapies, benefits, risks, and follow‑up schedules. Practical preparation makes the first appointment productive and sets a clear path forward.
Checklist items to prepare for a BHRT consult:
- Recent symptom diary and menstrual history
- Current medications and supplements
- Any prior hormone or metabolic lab results
- Your goals for therapy and questions about risks/benefits
Bringing these items enables a meaningful first step and helps your clinician design a targeted testing and treatment plan tailored to you. To schedule a consultation, contact Dr. Fred Bloem / Internal Healing and Wellness MD at the clinic phone number and be ready to discuss your history and goals during the initial visit.
Frequently Asked Questions
What lifestyle changes can support hormone balance alongside BHRT?
Lifestyle adjustments amplify BHRT’s benefits. Aim for a balanced diet rich in fiber and cruciferous vegetables to support estrogen metabolism, regular aerobic and resistance exercise to improve insulin sensitivity and body composition, and consistent sleep hygiene and stress‑management practices—like mindfulness or cognitive behavioral techniques—to reduce cortisol’s disruptive effects on reproductive hormones. These measures create a supportive foundation for hormone therapy to work more effectively.
How long does it typically take to see results from BHRT?
Some symptoms—particularly hot flashes and mood instability—often improve within a few weeks of starting BHRT. Sleep quality, energy, and cognitive changes may take several weeks to months as dosing and timing are refined. Bone and metabolic benefits develop over longer periods. Individual response varies, so regular follow‑up helps optimize timing and expectations.
Are there specific tests required before starting BHRT?
A comprehensive evaluation is essential before initiating BHRT. Targeted hormone testing may include blood, saliva, or urine panels timed to your cycle to measure estrogen, progesterone, and related markers. A thorough medical history and symptom review tailor the plan, and baseline screenings for cardiovascular and breast health may be recommended to ensure safety and guide hormone selection and delivery method.
What should I expect during my first BHRT consultation?
Your first BHRT visit will include a detailed review of symptoms, medical history, and treatment goals. The clinician will assess prior labs and current medications, recommend targeted hormone testing if needed, and outline potential therapies, benefits, risks, and follow‑up. This visit establishes a personalized roadmap for diagnosis, monitoring, and treatment.
Can BHRT help with weight management issues related to hormonal imbalance?
BHRT can support weight management when hormonal imbalance is a contributing factor. Estrogen and progesterone influence metabolism, appetite, and fat distribution, and restoring balance can improve energy and metabolic function. Sustainable weight management typically requires combining BHRT with lifestyle changes—nutrition, exercise, and sleep—to achieve long‑term results.
What are the differences between BHRT and traditional hormone replacement therapy (HRT)?
BHRT uses hormones chemically identical to those produced by the body, often derived from plant precursors. Traditional HRT may include synthetic hormones or animal‑derived preparations with different molecular structures. Because bioidentical hormones closely mimic endogenous hormones, they can offer more physiologic dosing and flexible routes. Discuss options with your provider to choose the safest, most effective approach for your needs.
How to Prepare for Your First Appointment with Dr. Bloem?
Prepare by collecting a symptom timeline, recent labs, a current medication and supplement list, and any relevant imaging or specialist notes. This information allows a focused initial assessment and efficient test ordering. Expect the clinician to review your history thoroughly, recommend cycle‑timed hormone testing when appropriate, and discuss provisional treatment pathways that may include BHRT and integrative supports. The clinic provides individualized testing plans and explains follow‑up so you understand monitoring cadence and therapeutic milestones.
Arriving prepared with documentation and clear goals speeds the path from evaluation to personalized treatment and makes the first visit an important step toward restoring estrogen and progesterone balance. For appointments and more information, call the clinic at (301) 260-2601 to arrange an initial consultation at the Kensington, MD location listed in practice information.
Conclusion
Bioidentical hormone replacement therapy (BHRT), when combined with personalized testing, monitoring, and targeted lifestyle and integrative supports, can meaningfully improve quality of life—relieving mood swings, sleep disturbances, and metabolic shifts tied to hormonal imbalance. Our approach emphasizes individualized care, patient education, and whole‑person strategies to support durable results. If you’re considering BHRT, schedule a consultation with our team to explore a plan tailored to your goals and health history. Take the first step toward restoring balanced hormones and better daily living today.



