PCOS Management Through Bioidentical Hormone Balance

PCOS Care Through Bioidentical Hormone Balance: Personalized, Integrative Solutions for Lasting Hormonal Health
Polycystic ovary syndrome (PCOS) is a multifaceted hormonal condition that affects reproductive, metabolic, and skin health. Modern research shows PCOS results from interacting disruptions in androgens, insulin signaling, and estrogen/progesterone balance, producing irregular cycles, ovulatory difficulties, acne, excess hair, and metabolic risk. This article outlines how restoring hormonal balance—especially with targeted bioidentical hormone replacement therapy (BHRT) used alongside tailored lifestyle and supplement strategies—can reduce symptoms, support fertility when desired, and improve metabolic markers. You’ll find clear explanations of the primary hormonal drivers of PCOS, how BHRT differs from conventional approaches, evidence-based adjuncts, answers to common patient questions, and practical next steps for a personalized plan. A note on clinical approach: Internal Healing and Wellness MD emphasizes root-cause assessment and individualized, integrative protocols that pair hormonal therapy with metabolic and lifestyle care to support long-term wellness. The section that follows describes the main hormonal imbalances that guide BHRT and adjunctive treatment choices.
Key Hormonal Imbalances in PCOS
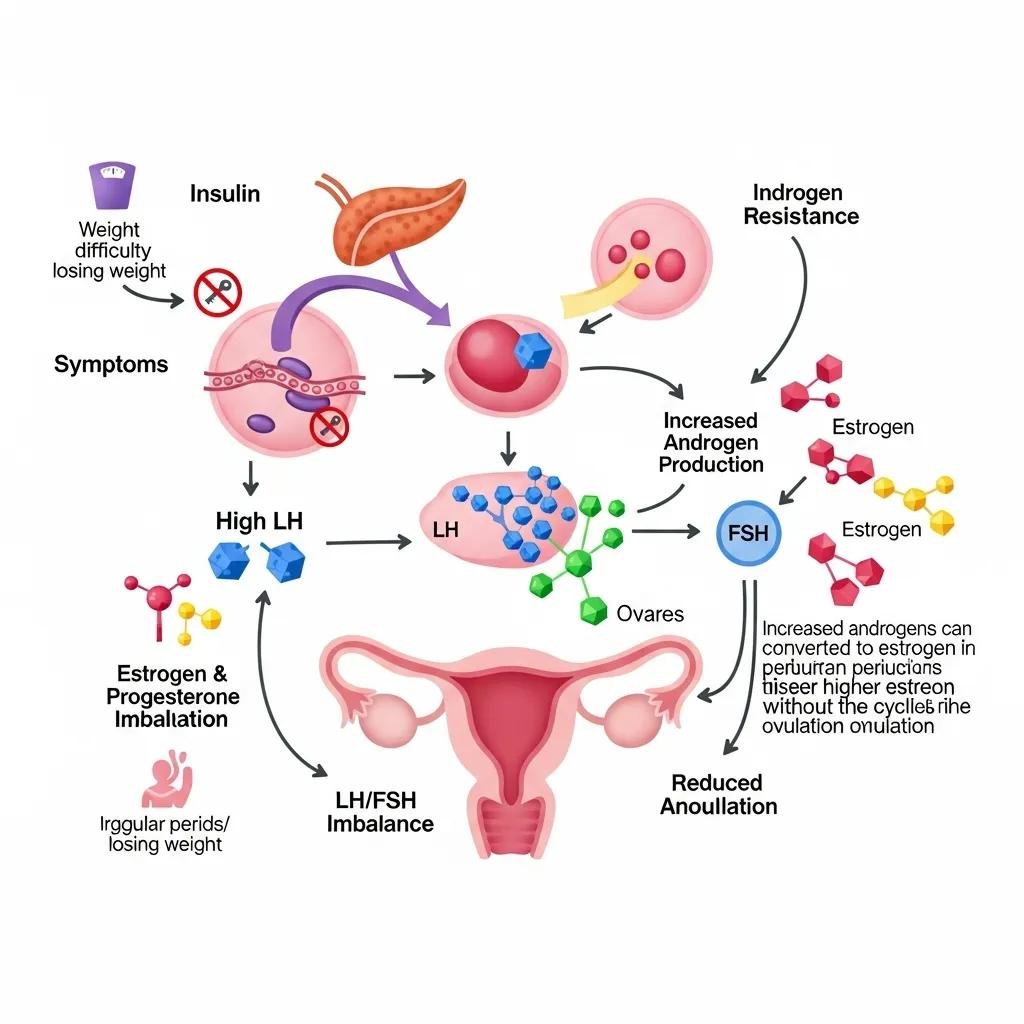
The core hormonal disturbances in PCOS are androgen excess, insulin resistance, and a disrupted estrogen–progesterone relationship. Each creates distinct symptoms and identifies actionable treatment targets. Excess androgens from ovarian and adrenal sources cause acne, increased hair growth, and follicle arrest; insulin resistance amplifies ovarian androgen production and raises cardiometabolic risk; and relative progesterone deficiency from anovulation leads to irregular bleeding and prolonged estrogen exposure. Mapping hormones to clinical signs helps clinicians and patients prioritize testing and create combined metabolic plus hormone-directed strategies. This framework also explains how BHRT and integrative measures can restore cycle patterns and metabolic balance.
Different hormonal signals in PCOS point to practical intervention options and recognizable symptom patterns.
| Hormone | Typical Imbalance Pattern | Clinical Signs / Targeted Intervention |
|---|---|---|
| Androgens (testosterone, DHEA-S) | Increased ovarian or adrenal production, often driven by LH and insulin | Acne, hirsutism, anovulation → focus on metabolic control, anti-androgen strategies, and selective hormonal modulation |
| Insulin | Peripheral insulin resistance with compensatory hyperinsulinemia | Weight gain, dyslipidemia, higher ovarian androgen synthesis → prioritize diet/exercise, insulin-sensitizing supplements and interventions |
| Estrogen | Variable; frequently unopposed or relatively elevated at times | Heavy or irregular bleeding, endometrial proliferation risk → balance with progesterone support and cycle regulation |
| Progesterone | Relative deficiency due to chronic anovulation | Irregular cycles, luteal phase insufficiency → target luteal support, timed progesterone therapy, and ovulation-promoting strategies |
This hormone-to-symptom mapping underscores why metabolic and endocrine treatments should be combined when planning BHRT.
How Estrogen and Progesterone Imbalances Affect PCOS Symptoms
In PCOS, progesterone is often low because ovulation is infrequent, while estrogen exposure can be intermittent and unopposed. Progesterone normally stabilizes the uterine lining, supports regular shedding, and tempers estrogen-driven growth; without it, patients can experience irregular bleeding, amenorrhea, and, over time, increased endometrial risk. Clinicians use cycle history, mid-luteal progesterone checks, and luteal metrics to identify these patterns and time replacement appropriately. Cyclic progesterone often improves menstrual regularity, lowers endometrial risk, and can indirectly reduce androgen-driven symptoms by normalizing feedback loops. These cycle-focused steps lead naturally into how a tailored BHRT plan restores these hormone relationships.
The Role of Androgen Excess and Insulin Resistance in PCOS
Androgen excess and insulin resistance form a reinforcing loop: high insulin levels boost ovarian theca cell androgen production, which worsens follicular arrest and anovulation. Hyperinsulinemia also lowers hepatic SHBG, increasing free androgens that show up as acne, excess hair, and central weight gain. Simple metabolic measures—fasting insulin, glucose, and HOMA‑IR—give actionable data to guide insulin-sensitizing strategies alongside hormone treatments. Treating insulin resistance is therefore essential to reduce both metabolic risk and the androgenic drive that blocks ovulation. Effective care couples metabolic interventions with direct androgen- and cycle-modulating therapies to interrupt this cycle and restore reproductive function.
How Bioidentical Hormone Replacement Therapy Supports PCOS Care
Bioidentical hormone replacement therapy (BHRT) uses hormones that match human molecules to correct specific deficits and rebalance endocrine feedback in PCOS. BHRT can supply cyclic progesterone to restore luteal support, employ transdermal estradiol or other estrogen-modulating approaches to coordinate cycles, and—selectively—use very low-dose bioidentical testosterone in cases where metabolic or sexual health goals warrant it. Personalization and close monitoring are essential: dose, formulation, and delivery route affect metabolic and dermatologic outcomes, and therapy must be integrated with insulin-sensitizing measures. The table below compares common bioidentical hormones by mechanism, formulation options, and PCOS-relevant considerations to support shared decision-making and follow-up planning.
Comparing bioidentical hormones clarifies mechanisms and trade-offs relevant to symptom control and metabolic safety in PCOS.
| Hormone | Mechanism | Formulations / PCOS Considerations |
|---|---|---|
| Bioidentical Progesterone | Re-establishes luteal support and opposes endometrial overgrowth | Micronized oral, vaginal suppository, topical — reduces endometrial risk and helps normalize bleeding patterns |
| Bioidentical Estradiol | Replaces or modulates estrogen signaling to coordinate cycles | Transdermal patches or gels often preferred to limit first-pass hepatic effects; dosing should account for insulin and androgen status |
| Bioidentical Testosterone | Can support libido and lean mass when deficient; influences metabolic tone | Used cautiously at low doses and only for selected patients; monitor for androgenic side effects given baseline hyperandrogenism in PCOS |
These comparisons emphasize why BHRT must be individualized and regularly reassessed to maximize benefit and limit risk.
When integrated with lifestyle and metabolic care, BHRT can provide several targeted benefits for people with PCOS:
- Cycle Regulation: Cyclic progesterone restores luteal support and can help normalize bleeding patterns.
- Skin and Hair Improvements: Hormone modulation plus metabolic interventions can reduce the endocrine drivers of acne and unwanted hair growth.
- Improved Symptoms and Quality of Life: Thoughtful hormone balancing supports mood, energy, and sexual health as part of a comprehensive plan.
Together, these outcomes show how BHRT works alongside metabolic therapies to deliver broader symptom relief and better reproductive results.
What Makes Bioidentical Hormones Different from Synthetic Options?
Bioidentical hormones are molecularly identical to the hormones produced by the body, which often leads to predictable receptor interactions and physiological responses. By contrast, some synthetic hormones have structural differences that change metabolism and receptor behavior. Delivery matters: transdermal, oral, topical, and vaginal routes differ in how much hepatic first-pass metabolism they cause and how they affect markers like SHBG and triglycerides—transdermal options often minimize hepatic effects and are chosen when metabolic safety is a priority. Limitations include variability in compounding and the need for evidence-based dosing; safe use depends on thoughtful lab monitoring and clinical follow-up. Knowing these differences helps patients and clinicians select formulations that align symptom goals with metabolic and reproductive safety.
How BHRT Helps Irregular Periods and Acne
BHRT improves cycle irregularity mainly by providing cyclic progesterone to restore luteal function or mimic its effects, producing more predictable bleeding and protecting the endometrium from unopposed estrogen. For acne and excess hair, correcting estrogen/progesterone balance and addressing metabolic drivers reduces free androgen activity and sebum production, often yielding clearer skin over weeks to months. In practice, many patients with anovulatory cycles see menstrual regularity within 2–3 cycles of tailored progesterone plus insulin-sensitizing care; dermatologic improvements typically take 8–12 weeks. BHRT is most effective when used as part of an integrated plan that treats both hormonal signals and metabolic contributors.
Why Personalized BHRT Protocols Matter in PCOS
PCOS is heterogeneous, so BHRT must be tailored to each person’s lab results, symptoms, fertility plans, and metabolic profile. Personalization starts with comprehensive testing and symptom mapping, then proceeds with careful dosing, delivery selection, and scheduled monitoring to optimize outcomes and limit side effects. Shared decision-making is core: patient priorities (fertility, cycle control, metabolic health) shape the treatment plan and follow-up schedule. This individualized approach positions BHRT as a durable part of an integrative pathway rather than a short-term fix.
Integrative and Holistic Therapies That Complement BHRT

Integrative therapies strengthen BHRT results by addressing insulin resistance, inflammation, and lifestyle factors that drive PCOS. Diets emphasizing low glycemic load or Mediterranean-style patterns improve insulin sensitivity and lipid patterns and help reduce androgenic drive when paired with weight management. An exercise plan that combines resistance training with moderate aerobic work enhances glucose handling and body composition, improving hormonal responsiveness. Stress reduction, sleep optimization, and gut-supportive measures further influence endocrine and inflammatory pathways relevant to PCOS. The table below summarizes key supplements and dietary strategies with their mechanisms, evidence strength, and practical dosing to help clinicians and patients choose effective adjuncts.
Targeting metabolic drivers with complementary therapies amplifies hormonal treatment and lowers the chance of symptom recurrence.
| Approach | Mechanism | Evidence / Typical Use |
|---|---|---|
| Inositol (myo-/D-chiro) | Improves insulin signaling and supports ovulation | Moderate evidence; common dosing 2–4 g/day; used to improve ovulatory frequency and metabolic markers |
| Berberine | Activates AMPK with effects similar to metformin on metabolism | Emerging to moderate evidence; typical dosing ~500 mg 2–3x/day; monitor for GI side effects |
| Omega-3 Fatty Acids | Anti-inflammatory effects and lipid improvement | Moderate evidence for reducing inflammation and improving lipids; dosing 1–3 g/day EPA/DHA |
| Low-GI / Mediterranean Diet | Blunts postprandial insulin spikes and supports weight management | Strong evidence for improving insulin sensitivity and cardiovascular risk; practical and sustainable for long-term adherence |
Practical lifestyle steps that consistently support hormonal balance include:
- Dietary Priorities: Emphasize low-GI carbohydrates, adequate protein, fiber-rich vegetables, and healthy fats to smooth blood sugar and reduce insulin peaks.
- Exercise Prescription: Combine resistance training two to three times weekly with about 150 minutes of moderate aerobic activity per week to improve insulin sensitivity and body composition.
- Stress and Sleep: Use relaxation practices, cognitive strategies, and steady sleep routines to lower cortisol-driven metabolic disruption.
How Diet, Exercise, and Stress Management Support Hormone Balance
Diet, exercise, and stress reduction target the metabolic core of PCOS by improving insulin sensitivity, lowering chronic inflammation, and restoring neuroendocrine balance that influences ovarian function. Low‑glycemic and Mediterranean-style diets moderate blood glucose and insulin responses, reducing ovarian androgen output and improving ovulation. Regular resistance and aerobic training increase muscle glucose uptake and favorably shift body composition, enhancing responsiveness to hormonal therapy. Managing stress and prioritizing sleep help normalize cortisol and autonomic tone, which otherwise worsen insulin resistance and reproductive dysfunction. When these pillars are in place, BHRT can work more effectively to restore cycle regularity and reduce androgen-driven symptoms.
Which Supplements Support Hormonal and Metabolic Health in PCOS?
Supplements with clinical support for PCOS focus on improving insulin signaling, lowering inflammation, and correcting common micronutrient gaps that can impair metabolism. Inositol (myo- and D‑chiro‑inositol) improves insulin signaling and ovulatory frequency and is a first-line adjunct for many patients. Berberine activates AMPK and can mimic some metabolic effects of metformin but may cause gastrointestinal symptoms in some people. Omega‑3s reduce inflammation and improve lipid profiles, indirectly helping androgen activity. Vitamin D and magnesium correct common deficiencies that can worsen metabolic measures. Use the earlier table and dosing guidance with clinical monitoring to select supplements safely.
How Dr. Fred Bloem’s Approach Enhances PCOS Outcomes
Internal Healing and Wellness MD follows a comprehensive integrative model that centers on root-cause evaluation and personalized protocols to improve outcomes in complex endocrine conditions such as PCOS. The practice offers extended visits, deep assessment, and individualized treatment plans that combine BHRT with metabolic, lifestyle, and supportive therapies. Core services include bioidentical hormone therapy, anti-aging and regenerative approaches, and care for complex chronic conditions. This framework enables careful BHRT titration within an integrative plan, paired with education and shared decision-making—factors that support better adherence and longer-term results.
This practice model naturally leads into patient-centered features and tailored care options for people seeking specialized PCOS management.
What Expertise and Patient-Centered Care Does Dr. Bloem Provide?
Dr. Fred Bloem’s model emphasizes longer visits, comprehensive histories, and personalized protocols for complex and chronic conditions, with BHRT used as one component of an integrative plan. Root-cause analysis helps clinicians reconcile labs, symptom clusters, and goals—whether fertility, cycle normalization, or metabolic improvement—before starting targeted therapies. Education and partnership are core: time is allotted to explain mechanisms, monitoring plans, and lifestyle measures that complement hormonal therapy. That individualized approach supports safe BHRT use by ensuring baseline testing, scheduled reassessments, and collaborative adjustments based on response and aims.
How Patient Education and Partnership Support Long-Term Wellness
Education and active partnership increase adherence, empower self-management, and help sustain lifestyle changes that reinforce hormone treatments over time. Structured touchpoints—baseline lab review, treatment planning, and follow-up visits—help patients understand how diet, exercise, supplements, and BHRT interact to produce results. Regular monitoring enables timely dose adjustments and minimizes side effects. When treatment aligns with patients’ priorities, they take greater ownership of the plan and maintain realistic expectations about timelines and milestones, all of which supports durable wellness gains.
Common Patient Questions About PCOS and Bioidentical Hormones
Patients frequently ask whether bioidentical hormones work for PCOS, how BHRT compares with standard treatments, and when to seek specialist care. Clear, evidence-aligned answers reduce uncertainty about monitoring, combined-therapy benefits, and realistic timelines for improvement. The FAQ below addresses safety, effectiveness, and next-step guidance to help people decide if BHRT within an integrative program fits their goals.
Can Bioidentical Hormones Help Manage PCOS Effectively?
Yes. When used as part of a comprehensive, individualized plan that treats metabolic drivers and matches patient goals, bioidentical hormones can effectively address specific PCOS symptoms. Progesterone replacement corrects luteal insufficiency and lowers endometrial risk, while careful estrogen management—often via transdermal routes—can support cycle coordination without worsening metabolic measures. BHRT complements, rather than replaces, insulin-sensitizing treatments, supplements, and lifestyle changes. Ongoing symptom tracking and lab monitoring are essential to confirm benefit and adjust therapy according to fertility goals and metabolic safety.
How Does BHRT Compare to Conventional PCOS Treatments?
BHRT focuses on restoring physiologic hormone patterns with molecules identical to endogenous hormones, whereas conventional options often use contraceptives or anti-androgens for symptom suppression. Oral contraceptives reliably control cycles and acne but may not improve insulin resistance; metformin targets metabolism but does not restore luteal progesterone. BHRT can be used alongside or instead of these approaches depending on goals—fertility support, cycle normalization, or symptom relief—but must be integrated thoughtfully with metabolic agents and closely monitored. Choice depends on individual priorities, risk profile, and clinician guidance.
Optimized PCOS Care with Personalized Bioidentical Hormones
Beginning PCOS care with an integrative, hormone-balanced plan follows a straightforward sequence: comprehensive assessment and labs, personalized BHRT plus metabolic plan design, initiation of lifestyle and supplement measures, and scheduled follow-up to refine treatment. This approach targets root contributors—insulin resistance and androgen excess—while using BHRT to correct cycle-specific deficits or symptom drivers. The checklist below helps patients prepare for a specialist consultation and understand the expected path of care.
- Comprehensive Assessment: Full medical history, symptom mapping, and baseline labs to define hormonal and metabolic patterns.
- Personalized Plan Development: Customized BHRT protocol with tailored supplement, diet, exercise, and stress-management recommendations aligned with your goals.
- Initiation and Monitoring: Start therapies with planned follow-ups and repeat labs to optimize dosing and track progress.
- Ongoing Adjustment: Titrate hormones and adjunctive therapies based on response, fertility planning, and evolving metabolic outcomes.
This stepwise path sets clear expectations and gives patients a measurable roadmap for progress.
What to Expect During a Consultation with Dr. Fred Bloem
A consultation with Dr. Bloem prioritizes extended visit time for a thorough history, root-cause evaluation, and a collaborative plan that blends BHRT with metabolic and lifestyle strategies. Expect detailed lab review, targeted diagnostic ordering when indicated, and a discussion of individualized BHRT options alongside diet, exercise, and supplement guidance. The visit will outline realistic timelines, monitoring schedules, and shared decisions about fertility or symptom-focused goals. Follow-up timing is set based on initial interventions, with the understanding that iterative adjustments are part of achieving long-term results.
How to Book a Personalized PCOS Treatment Plan at Internal Healing and Wellness MD
To start a personalized PCOS plan at Internal Healing and Wellness MD, bring a concise symptom history, any recent labs, and clear treatment goals—whether fertility, cycle control, or metabolic improvement—to your extended initial visit. Our model emphasizes longer consultations, patient education, and individualized protocols so clinicians can design BHRT and integrative plans that address each person’s root-cause drivers. Expect a structured first visit with comprehensive history-taking, focused lab review, and a clear plan for BHRT initiation and adjunctive therapies, plus scheduled follow-ups to track progress. This pathway is built for partnership and measurable movement toward hormonal balance and sustained wellness.
Frequently Asked Questions
What lifestyle changes can help manage PCOS symptoms effectively?
Practical lifestyle changes make a meaningful difference. Prioritize a low‑glycemic, fiber-rich diet with healthy fats and adequate protein to blunt insulin spikes. Regular physical activity that includes resistance training and aerobic work improves insulin sensitivity and body composition. Stress-reduction practices such as mindfulness, yoga, or breathing exercises, along with consistent sleep habits, help stabilize hormonal rhythms. These strategies, combined with medical treatments like BHRT when appropriate, improve symptom control and overall health.
How long does it typically take to see improvements with BHRT for PCOS?
Individual responses vary, but many patients notice changes within weeks to a few months. Menstrual regularity often improves within 2–3 cycles of targeted progesterone support, while dermatologic improvements such as clearer skin may take 8–12 weeks. Progress depends on baseline severity, adherence to lifestyle changes, and the specifics of the treatment plan. Regular follow-up lets your clinician adjust therapy to accelerate and sustain benefits.
Are there any risks associated with Bioidentical Hormone Replacement Therapy?
BHRT can be safe and effective, but no therapy is without risk. Potential side effects include mood changes, weight shifts, and, in some people, increased risks related to clotting or certain cancers depending on personal and family history. Thorough evaluation, individualized dosing, and routine monitoring are essential to minimize risk. A clinician-led, evidence-based plan helps ensure the benefits outweigh potential harms.
What role do supplements play in managing PCOS alongside BHRT?
Supplements can support metabolic and reproductive goals when paired with BHRT and lifestyle changes. Inositol helps insulin signaling and ovulation; omega‑3s reduce inflammation and improve lipids; berberine can offer metformin-like metabolic effects for some people; and vitamin D or magnesium may correct deficiencies that worsen metabolism. Use supplements thoughtfully within a monitored plan to ensure safety and avoid interactions.
How can I track my progress while undergoing treatment for PCOS?
Track menstrual patterns, symptom changes, and lab results to evaluate treatment progress. Keep a symptom diary to notice trends, and attend scheduled follow-ups for hormonal and metabolic testing. Recording diet, exercise, sleep, and stress-management habits can reveal how lifestyle adjustments influence outcomes. A structured monitoring plan helps your clinician tailor therapy and keeps progress measurable.
What should I discuss during my first consultation for PCOS management?
Share your medical history, current symptoms, previous treatments, and any recent lab results. Describe your goals—fertility, cycle regularity, symptom relief, or overall metabolic health—and ask about treatment options, monitoring plans, and timelines for expected improvements. Open communication helps build a personalized plan that aligns with your priorities.
Conclusion
Restoring hormonal balance with bioidentical hormone therapy—when combined with targeted lifestyle changes and appropriate supplements—can meaningfully improve cycle regularity, reduce androgenic symptoms, and enhance overall well-being for people with PCOS. This integrative, individualized approach addresses root causes rather than simply masking symptoms, empowering patients to take control of their health. To explore a tailored plan, schedule a consultation with our team and begin a measured, evidence-informed path toward hormonal harmony and lasting wellness.



