Integrative Support for Long COVID Symptoms

Integrative Long COVID Care: Personalized support for post‑viral fatigue and brain fog
Long COVID describes a set of lingering symptoms that persist or appear after the acute phase of SARS‑CoV‑2 infection. Rather than a single organ problem, most cases involve multi‑system imbalance—immune activation, mitochondrial energy shortfalls, autonomic dysfunction, and sometimes lingering viral fragments all play roles. This article outlines an integrative, functional medicine approach that seeks root causes, applies targeted therapies, and supports a stepwise, sustainable recovery for people with post‑viral fatigue and cognitive fog. Read on to learn how to recognize common Long COVID patterns, understand the underlying biology, and review evidence‑informed options such as IV nutrient support, hormone assessment, regenerative and ozone therapies, and individualized care planning. Below we unpack symptom clusters and mechanisms, describe the functional medicine evaluation and treatment framework, compare IV and regenerative approaches, and explain how clinicians build personalized protocols and monitor outcomes.
What are the key symptoms and likely drivers of Long COVID?
Long COVID most often shows up as a constellation of persistent complaints lasting weeks to months after the initial infection. These reflect systemic dysregulation rather than a single, isolated injury. Mechanisms frequently involved include ongoing immune activation, reduced mitochondrial ATP production, autonomic nervous system instability, and intermittent viral antigen persistence. Together these lower physiologic reserve and cognitive bandwidth, producing fatigue, brain fog, and limited exercise tolerance. Clinically, identifying symptom clusters matters because treatment differs depending on whether immune, metabolic, autonomic, or endocrine processes are dominant. Below we list cardinal symptoms and then connect them to common mechanistic drivers so you can see how targeted testing shapes personalized care.
Which symptoms most commonly point to Long COVID? The clusters below help clinicians separate post‑viral syndromes from simple deconditioning.
- Persistent, daily fatigue that interferes with work and routine activities.
- Cognitive dysfunction — memory lapses, slowed thinking, and trouble concentrating.
- Post‑exertional malaise: symptom worsening after physical or mental effort.
These core problems frequently occur alongside shortness of breath, heart palpitations, orthostatic intolerance, sleep disruption, and mood changes. Mapping these clusters guides focused testing for immune markers, mitochondrial function, and autonomic stability, which then directs individualized treatment choices.
Which post‑viral fatigue and brain fog symptoms suggest Long COVID?
In Long COVID, post‑viral fatigue and brain fog present as sustained low energy and slowed cognitive processing that are out of proportion to activity. Patients often describe difficulty concentrating at work, short‑term memory gaps, and a feeling that thinking is sluggish—symptoms that interfere with complex tasks and social life. Urgent red flags include progressive neurological changes, new focal weakness, severe orthostatic intolerance with fainting, or rapidly worsening breathing—these require immediate specialist referral. For milder presentations, clinicians look for a pattern of post‑exertional symptom flares, disrupted sleep, and fluctuating cognition that worsen with stress or activity. Recognizing that pattern helps prioritize autonomic testing, metabolic labs, and neurocognitive assessment to distinguish Long COVID from primary psychiatric conditions or simple deconditioning and to allow more precise treatment planning.
How do immune imbalance and mitochondrial dysfunction fuel Long COVID?
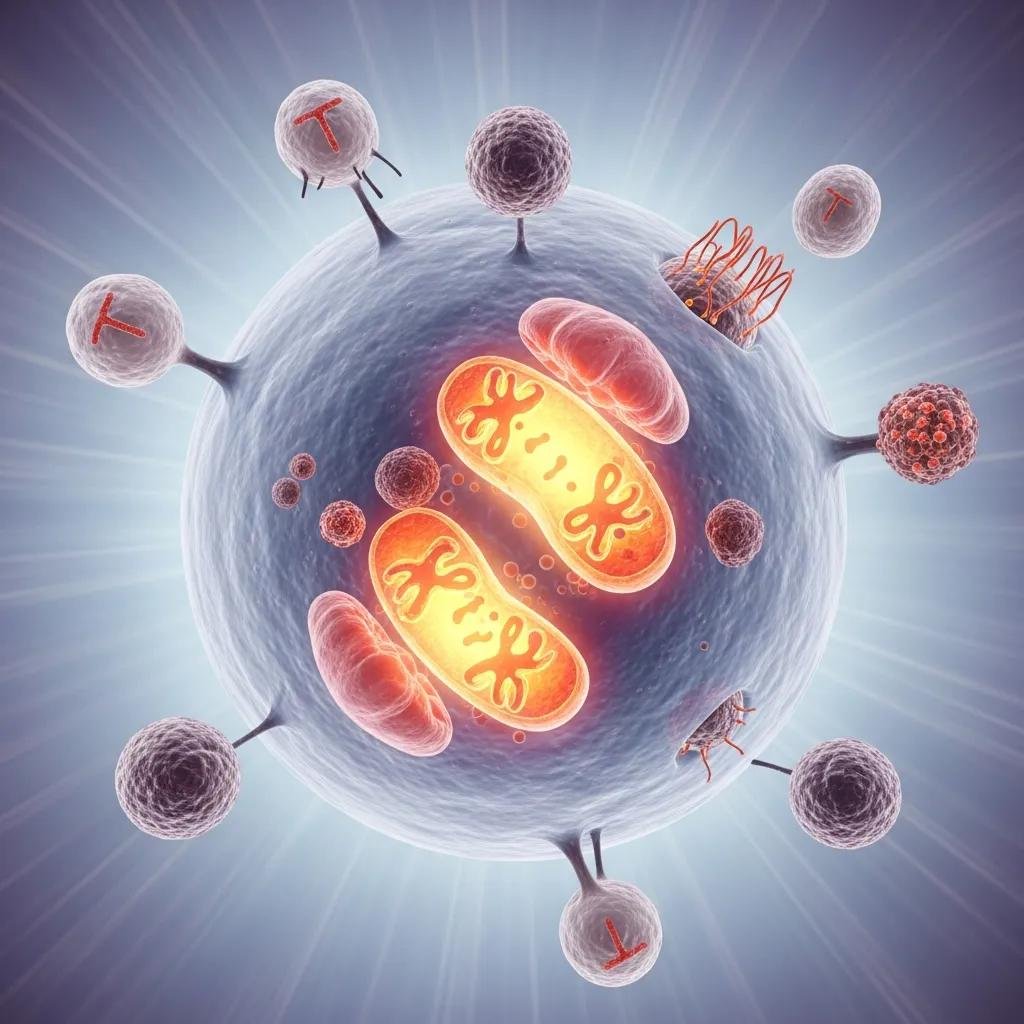
Immune dysregulation in Long COVID often shows as low‑grade inflammation, altered cytokine signaling, and immune cell exhaustion, creating a sustained inflammatory environment that affects brain and muscle function. Chronic immune activation can disrupt synaptic signaling and neurotransmitter balance, producing cognitive and mood symptoms, while increased oxidative stress damages mitochondrial components. Mitochondrial dysfunction lowers cellular ATP production and limits energy available to muscles and neurons, contributing to profound fatigue and exercise intolerance. Studies through 2020–2023 reveal overlaps between Long COVID and other post‑infectious fatigue syndromes, underscoring the need for therapies that reduce inflammation, restore mitochondrial function, and bolster antioxidant defenses. Linking these mechanisms to targeted interventions—antioxidants, NAD+ and cofactor support, immune‑modulating ozone approaches, and autonomic rehabilitation—creates a cohesive, root‑cause treatment pathway rather than simply masking symptoms.
How does functional medicine support Long COVID recovery?
Functional medicine applies a root‑cause framework to Long COVID by systematically assessing physiologic dysfunction, tailoring targeted interventions, and tracking objective and patient‑reported outcomes over time. In practice, clinicians first evaluate immune markers, metabolic and mitochondrial function, hormonal status, autonomic balance, and potential infectious or toxic contributors; next they apply personalized treatments—nutrient repletion, IV support, immune modulation, and practical lifestyle prescriptions; finally they monitor progress and refine the plan through scheduled reassessments. This Assess → Treat → Support approach helps teams prioritize interventions most likely to improve energy, cognition, and daily function. The table below links common diagnostic tools to their clinical purpose and typical therapeutic outcomes so you can see how testing guides treatment selection.
Functional assessment tools map directly to targeted therapies and measurable outcomes.
| Diagnostic Tool | Purpose | Typical Treatment Mapping |
|---|---|---|
| Autonomic testing (tilt, HRV) | Detect orthostatic intolerance and vagal dysfunction | Autonomic retraining, tailored fluid/salt plans, activity pacing |
| Mitochondrial/metabolic labs | Identify impaired ATP production and nutrient gaps | NAD+ support, CoQ10, B‑vitamins, individualized nutrition |
| Inflammatory and immune panels | Uncover chronic immune activation or post‑infectious autoimmunity | Immune modulation, antioxidants, precision supplements |
That mapping shows how a focused diagnostic evaluation translates to prioritized therapies and measurable recovery goals, and it sets up the root‑cause treatments described below.
What personalized root‑cause treatments does functional medicine offer?

Functional medicine weaves nutrient repletion, mitochondrial support, and immune‑modulating strategies into individualized protocols guided by testing. Common interventions include NAD+ replenishment and cofactor replacement to restore cellular energy, antioxidant therapy such as glutathione to lower oxidative stress, and targeted immune modulation when ongoing inflammation is present. Clinicians also prioritize sleep restoration, graded activity with careful pacing to avoid post‑exertional malaise, and autonomic rehabilitation for orthostatic symptoms. Lab‑guided dosing and iterative monitoring let teams safely intensify or taper interventions in response to objective improvement, maximizing the chance of meaningful symptom reduction.
What personalized root‑cause treatments does functional medicine offer?
Personalized root‑cause care targets the physiologic drivers revealed by diagnostic testing and adapts as patients respond. For mitochondrial insufficiency, typical strategies combine NAD+ support with CoQ10, L‑carnitine, and B‑vitamins to support ATP production and cellular respiration. For immune imbalance, clinicians may use antioxidant IVs, ozone‑based immune modulation, and targeted supplementation to rebalance cytokine activity. Lifestyle prescriptions—sleep optimization, anti‑inflammatory nutrition, paced breathwork, and graded activity—support recovery and lower relapse risk. These elements form a multi‑domain protocol that is refined at follow‑up visits to align treatments with measurable gains in energy, cognition, and daily function.
How does integrative medicine enhance holistic COVID recovery?
Integrative medicine layers complementary therapies—neural therapy, mind‑body practices, acupuncture, and targeted regenerative injections—onto functional protocols when symptoms resist single‑modality care. Local injections and neural techniques can ease muscle and joint pain that limit activity, while mind‑body work and breathing practices improve autonomic balance and reduce symptom amplification. This multimodal approach builds resilience by addressing physical, neuroimmune, and psychosocial drivers of Long COVID, and it’s delivered within longer, relationship‑based visits that emphasize education and pacing. When combined with biomarker‑guided medical therapies, integrative care often improves adherence and functional gains by treating the whole person rather than isolated complaints.
Unlocking Personalized Solutions for Long COVID Recovery
IV therapies deliver concentrated antioxidants, cofactors, and immune‑support nutrients directly into the bloodstream to more rapidly address oxidative stress, mitochondrial substrate deficits, and immune dysfunction. Key IV options used in post‑viral recovery include glutathione for antioxidant and detox support, high‑dose vitamin C for oxidative stress reduction and immune modulation, and NAD+ infusions aimed at restoring critical mitochondrial coenzymes and supporting cognitive energy. These therapies are usually part of a broader program—nutritional repletion, hormone optimization, autonomic rehabilitation—not standalone fixes. The table below summarizes common IV options by mechanism, clinical use‑case in Long COVID, and target symptoms to support patient‑clinician decision making.
The following comparison clarifies IV mechanisms, indications, and expected symptom targets.
| IV Option | Mechanism | Symptom Targets |
|---|---|---|
| Glutathione IV | Intracellular antioxidant that supports detox and mitochondrial enzymes | Fatigue, oxidative‑related brain fog, muscle aches |
| High‑dose Vitamin C IV | Powerful antioxidant and immune‑modulating nutrient | Inflammation‑related fatigue and immune imbalance |
| NAD+ IV | Repletes NAD+ to support mitochondrial ATP production | Mental clarity, processing speed, overall stamina |
How do glutathione, vitamin C, and NAD+ IV treatments help recovery?
Each IV agent supports distinct biochemical pathways: glutathione neutralizes reactive oxygen species and aids cellular detox, vitamin C limits oxidative injury and supports immune cells, and NAD+ replenishment restores a coenzyme central to mitochondrial respiration and DNA repair. Clinically, protocols often begin with an induction series of treatments then move to maintenance dosing based on symptom response and lab markers. Plans are individualized to avoid overuse and to integrate safely with hormones or regenerative therapies. When combined with lifestyle changes and careful monitoring, IV therapies can accelerate biochemical recovery and help sustain functional gains.
How do glutathione, vitamin C, and NAD+ IV treatments help recovery?
Glutathione, vitamin C, and NAD+ each target pathways implicated in Long COVID and together form a complementary IV toolkit. Glutathione serves as the primary intracellular antioxidant, protecting mitochondrial enzymes and neural signaling—changes that often translate into improved energy and clarity. Vitamin C acts both as an antioxidant and an immune‑supportive micronutrient, helping to modulate inflammatory cascades that sustain fatigue. NAD+ supports enzymes involved in ATP production and cellular repair, which can improve mental endurance and sustained energy when deficiency contributes. Used judiciously and with monitoring, these IV options can restore biochemical capacity while other modalities rebuild physiologic resilience.
What role does detoxification play in relieving post‑viral symptoms?
Detoxification strategies aim to lower toxin burden and oxidative drivers that may prolong immune activation and metabolic stress after viral illness. Common modalities include IV antioxidant regimens, ozone therapies, and—when indicated—extracorporeal approaches. Thoughtful detox can reduce inflammatory load and support mitochondrial recovery, but it requires targeted testing and careful monitoring to avoid nutrient depletion or overtaxing fragile physiology. Safety measures include gradual implementation, electrolyte and nutrient checks, and pausing detox during acute flares or infections. Clinicians favor evidence‑based, tolerable approaches rather than aggressive regimens. When detox is integrated into a comprehensive plan—paired with mitochondrial support, sleep restoration, and pacing—it can lower symptom burden and improve rehabilitation readiness.
How can hormone balance improve fatigue and mood in Long COVID?
Hormonal imbalances—affecting thyroid function, sex hormones, or adrenal regulation—can worsen fatigue, sleep disruption, and mood symptoms after viral illness. Correcting documented deficiencies often enhances recovery. Hormones influence mitochondrial efficiency, circadian rhythms, and neurotransmitter balance, so restoring appropriate levels can boost energy production, sleep quality, and cognitive performance. A measured, lab‑guided approach to bioidentical hormone replacement can complement mitochondrial and immune‑targeted therapies, especially for patients with persistent, documented deficits. The table below compares common hormone strategies, expected benefits, and monitoring considerations to show how endocrine care fits into an integrated Long COVID plan.
| Hormone Strategy | Benefit | Monitoring Considerations |
|---|---|---|
| Bioidentical sex hormones | Improve energy, mood, and sleep when deficiency is present | Baseline hormone panels, symptom tracking, periodic labs |
| Thyroid optimization | Restore metabolic rate and cognitive clarity | TSH, free T4/T3, and clinical symptom review |
| HPA/adrenal support | Stabilize daily energy rhythms and stress response | Cortisol rhythm testing and symptom diaries |
What are the benefits of bioidentical hormone replacement therapy?
When testing shows true deficiencies, bioidentical hormone replacement can improve daytime energy, mood regulation, and sleep quality—domains that strongly influence Long COVID recovery. Properly tailored hormone therapy can increase cognitive endurance and support restorative sleep cycles that aid tissue repair and mitochondrial recovery. Patient selection and careful dosing are essential; clinicians use serial labs and symptom metrics to titrate therapy and avoid overtreatment. Hormone optimization is most effective when combined with mitochondrial support, nutritional repletion, and autonomic rehabilitation, creating a synergistic foundation for restoring physiologic resilience.
How does hormone optimization support holistic symptom management?
Hormones affect multiple systems—mitochondrial function, inflammatory tone, and circadian regulation—so correcting hormonal deficits can produce broad gains in energy, cognition, and mood. In practice, hormone optimization reduces barriers to rehabilitation by improving sleep and metabolic flexibility, which makes graded activity and cognitive retraining more achievable. Coordinated care—linking hormones with IV support, ozone treatments, and lifestyle changes—ensures hormone therapy complements rather than replaces other recovery strategies. Close monitoring and collaboration with specialists when needed protect outcomes and let clinicians integrate endocrine care into a stepwise recovery plan.
What regenerative and ozone therapies support tissue repair and immune function?
Regenerative injections and ozone‑based therapies aim to restore tissue health, modulate immune responses, and improve microcirculation—effects that can benefit patients with post‑viral musculoskeletal pain, chronic inflammation, or microvascular complaints. Examples include Prolozone for localized tissue repair, major autohemotherapy (MAH) for systemic modulation, and extracorporeal blood ozone approaches that influence oxidative signaling pathways. Patient selection matters: these therapies have specific contraindications and should be performed by experienced proceduralists. The sections below describe how Prolozone works and outline the immune‑modulating rationale for ozone and MAH in Long COVID rehabilitation.
How does Prolozone therapy support joint and tissue regeneration?
Prolozone therapy stimulates localized repair by injecting a blend of oxygen and ozone into damaged ligaments, tendons, or joint spaces to provoke reparative cascades and reduce chronic inflammation. For patients whose post‑viral myalgias or joint pain limit rehabilitation, Prolozone can reduce pain and improve mobility, enabling better participation in physical therapy and graded exercise. Regimens vary by tissue and severity, and injections are combined with rehabilitative approaches—manual therapy and progressive loading—for lasting benefit. When paired with systemic anti‑inflammatory and mitochondrial support, local regenerative injections can speed return to activity and lower long‑term disability risk.
What immune modulation benefits come from ozone and major autohemotherapy?
Ozone therapies and major autohemotherapy deliver controlled oxidative stimuli that trigger antioxidant defenses, improve oxygen delivery, and shift inflammatory signaling toward resolution. The goal is to reduce pathological immune activation without broadly suppressing host defenses—useful for patients left with a persistent inflammatory signature after viral illness. Evidence supports careful adjunctive use of ozone modalities alongside other integrative treatments, with attention to contraindications and procedural safety. When used within a monitored, multimodal plan, ozone‑based approaches can improve circulation, lower inflammatory burden, and contribute to gains in fatigue and cognitive clarity.
Where can patients find personalized treatment plans and real‑world outcomes?
Patients seeking individualized care typically start with a comprehensive intake: detailed history, targeted laboratory testing, autonomic and functional assessments, and symptom mapping to prioritize treatment targets. Multidisciplinary plans then blend evidence‑based medical therapies, integrative procedures, and lifestyle prescriptions with regular follow‑up to measure progress and refine the protocol. Below we outline a typical care pathway and summarize common themes from patient experiences so you can see likely trajectories and next steps for arranging care.
How are individualized integrative care plans developed for Long COVID?
Individualized care begins with a thorough intake and focused testing to identify dominant drivers—mitochondrial insufficiency, immune dysregulation, autonomic dysfunction, or hormonal deficits. Clinicians prioritize interventions that address the most limiting issues first—for example, stabilizing autonomic function before advancing physical rehabilitation—and set measurable short‑term goals to track improvement. Follow‑up is scheduled to reassess labs, adjust supplements or therapies, and review symptom diaries so the plan evolves with the patient. Coordination with other specialists is arranged when needed, and practical education about pacing, sleep hygiene, and graded activity empowers patients to take an active role in recovery.
What do patient testimonials reveal about recovery experiences?
Anonymized patient stories commonly report gradual but meaningful improvement when care is individualized and multimodal. Themes include initial stabilization of energy and sleep, followed by incremental gains in cognitive clarity and exercise tolerance as mitochondrial and autonomic issues are addressed. Patients also note the importance of clinician time and clear education in preventing relapses and sustaining improvements. For those ready to pursue evaluation and personalized planning, booking a consultation with clinicians experienced in integrative Long COVID care—such as the team at Internal Healing and Wellness MD—offers a practical next step toward a measured, test‑guided recovery pathway.
If you’re ready to pursue a tailored evaluation, schedule a consultation with Dr. Fred Bloem at Internal Healing and Wellness MD in Kensington, MD. Initial visits provide ample time for thorough history‑taking, targeted testing, and collaborative planning to prioritize interventions that match your symptom drivers and recovery goals. The clinic integrates functional and integrative modalities—IV therapies, hormone evaluation, regenerative injections, and ozone options—into personalized plans, with clear monitoring and follow‑up to track outcomes and refine therapy over time.
Frequently Asked Questions
What lifestyle changes can support recovery from Long COVID?
Simple, sustainable lifestyle changes can meaningfully support recovery. Prioritize consistent sleep habits, gentle and paced physical activity, and an anti‑inflammatory diet based on whole foods. Mind‑body practices—meditation, breathwork, and gentle yoga—help manage stress and reduce symptom amplification. Stay well hydrated and limit excessive caffeine and alcohol. Work with your care team to tailor these steps so they support your specific recovery plan.
How long does it typically take to recover from Long COVID?
Recovery timelines vary widely. Some people notice steady improvement within weeks; others need months or longer. Progress is often non‑linear, with good days and setbacks. Factors that influence recovery include initial illness severity, pre‑existing health conditions, and dominant symptom drivers. Ongoing monitoring and a structured, individualized rehabilitation plan help produce more consistent gains over time.
Are there specific dietary recommendations for Long COVID patients?
Diet can play an important role. Focus on antioxidant‑rich fruits and vegetables, healthy fats (like omega‑3s), lean proteins, and whole grains to support inflammation control and cellular repair. Limit processed foods, added sugars, and trans fats. Hydration matters. A nutritionist experienced with post‑viral recovery can tailor recommendations to your labs and symptoms.
What role does mental health play in Long COVID recovery?
Mental health is central to recovery. Anxiety, depression, and cognitive symptoms commonly accompany physical complaints and can amplify disability. Integrating therapy, support groups, or mindfulness practices improves coping and resilience. Cognitive behavioral therapy (CBT) and other structured approaches can help patients develop practical strategies to manage symptoms and maintain progress.
How can patients track their symptoms effectively during recovery?
Consistent tracking helps both patients and clinicians see trends and guide adjustments. Keep a symptom diary noting daily energy, cognitive function, sleep, and activity tolerance. Mobile health apps can simplify this process. Regularly review entries with your provider to assess treatment response and refine the care plan.
What are the potential long‑term effects of Long COVID?
Long COVID can produce persistent fatigue, cognitive changes, respiratory problems, and sometimes musculoskeletal or cardiovascular symptoms. Research is ongoing, and while many people improve, a subset may experience prolonged health challenges. Early, targeted intervention and a comprehensive plan can reduce long‑term risk and support better outcomes.
Conclusion
Integrative Long COVID care combines root‑cause evaluation with multi‑modal, evidence‑informed therapies to address persistent fatigue and brain fog. By focusing on underlying drivers and delivering personalized, monitored interventions, patients can often regain energy, clarity, and function. If you need tailored support, a consultation with a qualified clinician is a practical first step. Explore our resources or contact the clinic to learn more about how integrative therapies can help your recovery journey.



