
Optimizing Cortisol Management: Strategies for Stress Resilience
Cortisol is a steroid hormone made by the adrenal glands that helps the body marshal energy, modulate inflammation, and align physiology with the sleep–wake cycle. This article breaks down cortisol’s roles, how the HPA axis controls its release, and why brief spikes versus long-term elevation matter for health. You’ll learn to spot signs of high cortisol, understand HPA feedback and adrenal function, and use evidence-based strategies—sleep, nutrition, movement, and stress-reduction—to lower cortisol naturally. We also clarify functional medicine perspectives on adrenal dysregulation and outline clinical options, like bioidentical hormone replacement and integrative supportive services, when supervised care is appropriate. Practical lists, comparison tables, and clear action steps will help you turn physiology into everyday choices for better stress resilience and hormonal balance.
What Is Cortisol and How Does It Affect the Body?
Cortisol is a glucocorticoid produced by the adrenal cortex that helps regulate metabolism, immune activity, and the body’s acute stress response. It mobilizes glucose, downregulates nonessential processes during stress, and shapes inflammatory signaling—actions that support short-term survival. Cortisol follows a daily rhythm: a morning peak to support waking and daytime energy, and a low point at night to allow sleep. When that rhythm is disrupted, people often notice fatigue, insomnia, or daytime brain fog. Grasping these basic functions makes it easier to see why timing and level determine whether cortisol is protective or harmful.
What Is Cortisol and Why Is It Called the Stress Hormone?
We call cortisol the “stress hormone” because it rises quickly in response to physical or psychological threats, providing fuel and focus for immediate action. In acute stress, cortisol increases blood sugar, shifts energy to critical systems, and tempers inflammation—useful short-term effects. When cortisol stays high over time, though, it creates allostatic load: metabolic and structural changes like central fat accumulation, insulin resistance, and altered neuronal sensitivity that raise long-term disease risk. The key is distinguishing adaptive short-term responses from maladaptive chronic exposure so interventions can restore balance.
How Does Cortisol Regulate the Body’s Stress Response and Circadian Rhythm?
Cortisol release is tied to the body’s circadian clock: levels rise before waking to support alertness and fall at night to help sleep onset. This link connects adrenal output with the suprachiasmatic nucleus and peripheral clocks so cortisol both signals and responds to behavior, light, and sleep. When sleep is shortened or circadian cues are disrupted—think shift work or late-night screens—cortisol rhythms can flatten or shift, causing daytime fatigue and night-time arousal that perpetuate dysregulation. Reestablishing consistent sleep timing and daytime light exposure supports a healthier cortisol rhythm and improves stress resilience.
How Does the HPA Axis Control Stress and Cortisol Levels?
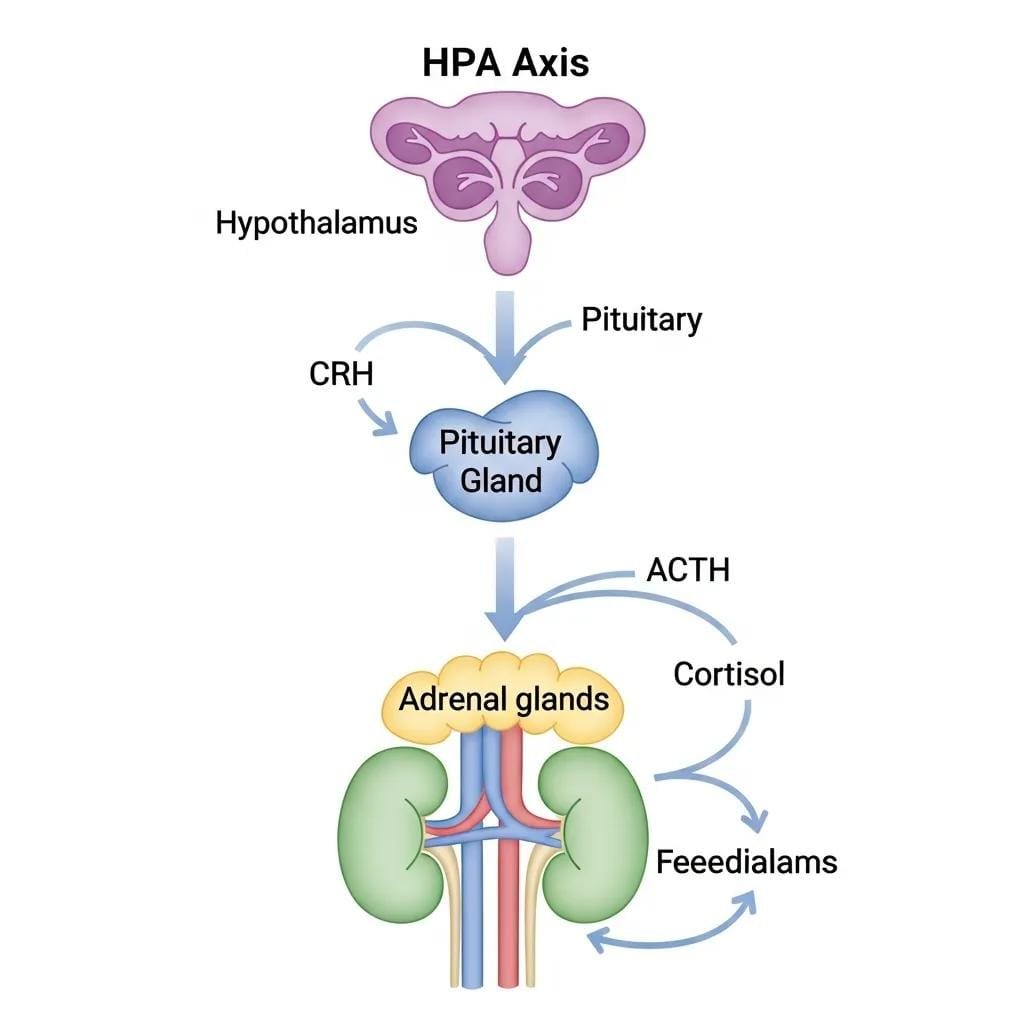
The hypothalamic-pituitary-adrenal (HPA) axis is the primary neuroendocrine pathway that controls cortisol through a stepwise signaling cascade and negative feedback. The hypothalamus releases corticotropin-releasing hormone (CRH), which tells the pituitary to secrete ACTH; ACTH then prompts the adrenal cortex to produce cortisol. Circulating cortisol feeds back to suppress CRH and ACTH, keeping levels in a functional range. Persistent stress or chronic inflammation can shift set points and blunt feedback. Understanding the HPA axis explains why psychological state, autonomic tone, and systemic inflammation all shape cortisol output.
What Is the Hypothalamic-Pituitary-Adrenal Axis and Its Function?
The HPA axis is a three-level communication system—hypothalamus → pituitary → adrenal—that translates neural and emotional signals into hormonal action. CRH from the hypothalamus stimulates pituitary receptors to release ACTH, which increases cortisol synthesis in the adrenal cortex; cortisol then affects metabolism, immunity, and many other systems. Clinically, HPA dysfunction can show up as abnormal cortisol rhythms, failure to suppress with dexamethasone, or blunted stimulation responses—each pointing to different diagnostic paths. Thinking of the HPA axis as a feedback-regulated thermostat helps explain why both underactivity and overactivity produce distinct symptoms and treatment strategies.
How Does the Brain-Adrenal Connection Influence Cortisol Production?
The brain shapes cortisol because it interprets threats and activates HPA signaling through limbic and cortical pathways. Cognitive appraisals, emotional state, and learned responses influence CRH release, while sympathetic activation can amplify adrenal responsiveness through catecholamine interactions. Patterns like rumination, chronic worry, or hypervigilance sustain brain-driven HPA activation; conversely, cognitive-behavioral techniques and relaxation training can downregulate the circuit. This brain–adrenal dialogue shows why psychological and autonomic interventions are central to long-term cortisol control.
What Are the Symptoms and Health Effects of High Cortisol and Chronic Stress?
High cortisol and prolonged stress affect many organ systems and produce identifiable symptom clusters, from sleep disruption to metabolic and mood disorders. Elevated cortisol shifts energy toward glucose production and fat storage, suppresses some immune functions while promoting low-grade inflammation, and alters neurotransmitter systems that affect mood and cognition. Watch for patterns—progressive belly weight gain, persistent anxiety, and fragmented sleep—that suggest chronic dysregulation and merit further evaluation. The table below summarizes common system effects and clinical examples to help distinguish acute stress from chronic cortisol-driven conditions.
Different systems show characteristic changes when cortisol is persistently elevated:
| System Affected | Physiological Effect | Clinical Examples |
|---|---|---|
| Metabolic | Increased gluconeogenesis and insulin resistance | Central weight gain, elevated fasting glucose |
| Cardiovascular | Raised blood pressure and vascular tone | Hypertension, increased heart rate |
| Immune | Suppressed adaptive immunity with low‑grade inflammation | Frequent infections, persistently elevated inflammatory markers |
| Neuropsychiatric | Neurotransmitter changes and hippocampal effects | Anxiety, depression, memory or focus complaints |
What Are Common Symptoms of High Cortisol and Adrenal Imbalance?
Typical signs of sustained high cortisol include ongoing fatigue despite sleep, disproportionate belly fat, trouble sleeping with early-morning awakenings, mood swings or anxiety, and cognitive fog. You may notice skin thinning, easy bruising, menstrual changes, increased carb cravings, or reduced exercise tolerance. Some cases indicate primary endocrine disease and need formal testing; others reflect functional dysregulation that often responds to lifestyle and integrative measures. Tracking symptom clusters and their course helps decide whether testing (for example, salivary cortisol panels or morning cortisol) or trial interventions are appropriate.
How Does Chronic Stress Impact Metabolism, Immunity, and Mental Health?
Chronic stress sustains cortisol-driven shifts—insulin resistance and visceral fat gain—by keeping glucose mobilized and altering appetite hormones. Immune effects can be mixed: some defenses are suppressed while other inflammatory pathways remain active, contributing to autoimmune risk and slower recovery from infections. Mental health consequences include increased anxiety, depressive symptoms, and impairments in memory and executive function tied to cortisol’s effects on the hippocampus and prefrontal cortex. These intersecting pathways explain why long-term stress raises the risk for metabolic syndrome, heart disease, and mood disorders, and why recovery usually requires a multi-modal approach.
How Can You Naturally Lower Cortisol and Manage Stress Effectively?

Evidence-based, practical strategies can lower cortisol naturally by stabilizing circadian cues, improving metabolic control, and reducing perceived stress. Interventions that consistently change physiology—regular sleep timing, balanced meals to avoid blood-sugar dips, moderate exercise with adequate recovery, and daily stress-reduction habits—reduce HPA activation and help reestablish healthier cortisol rhythms. Below are structured, actionable steps plus a comparison table to guide realistic implementation and set expectations for measurable improvement over weeks to months.
Core lifestyle interventions to lower cortisol include the following:
- Sleep Optimization: Keep regular sleep–wake times and create a cool, dark bedroom to support restorative sleep.
- Balanced Nutrition: Stabilize blood sugar with protein, fiber, and healthy fats at regular intervals.
- Appropriate Exercise: Mix moderate aerobic work and resistance training with restorative movement to avoid overtraining.
- Mindfulness and Relaxation: Daily breathwork, meditation, or progressive muscle relaxation reduces physiological reactivity.
These foundations support hormonal balance and make patients better candidates for any additional clinical or integrative therapies when needed.
The following table contrasts common interventions with their mechanisms and practical recommendations:
| Intervention | Mechanism | Practical Recommendation |
|---|---|---|
| Sleep Hygiene | Re‑entrains circadian cortisol rhythm | Fixed sleep schedule; aim for 7–9 hours nightly |
| Low-Glycemic Meals | Limits glucose spikes and cortisol demand | Include protein and fiber at meals; avoid late-night carbs |
| Regular Moderate Exercise | Builds metabolic resilience and lowers baseline cortisol | 30–45 minutes, 3–5× per week; include strength training |
| Mindfulness Practices | Engages parasympathetic tone to lower HPA activity | 10–20 minutes daily of meditation or focused breathing |
People who consistently apply these changes often notice better sleep and daytime energy within 2–6 weeks; metabolic and mood improvements commonly follow within 8–12 weeks with continued practice.
At Internal Healing and Wellness MD (Dr. Fred Bloem), patients with more complex needs can access integrative, supervised protocols that complement lifestyle change. Our practice focuses on root-cause assessment, longer visits for a thorough evaluation, and clinic options—such as IV nutrient support and targeted detoxification—when clinically indicated. If symptoms persist or you want supervised adjunctive care, schedule a consult to discuss individualized next steps.
What Role Does Adrenal Health Play in Stress and Hormonal Balance?
Adrenal function is central to stress physiology, but the language matters: adrenal insufficiency is a defined endocrine disorder, while “adrenal fatigue” is a term used in integrative medicine to describe chronic dysregulation without clear gland failure. Functional medicine evaluates adrenal health using symptom patterns, circadian testing (for example, serial salivary cortisol), and a broader look at autonomic and metabolic contributors rather than relying on a single serum cortisol. Clear distinctions help patients know when endocrine referral is needed and when targeted lifestyle and integrative therapies may offer benefit.
How Does Functional Medicine View Adrenal Fatigue and Insufficiency?
Functional medicine separates true adrenal insufficiency—diagnosed with specific cortisol thresholds and stimulation tests—from patterns where cortisol rhythms are blunted or inverted but not critically low. Practitioners take detailed histories, use serial measures like salivary or hair cortisol when appropriate, and evaluate related systems such as thyroid function and sleep. The aim is to identify drivers—sleep loss, chronic infection, nutrient gaps, or psychosocial stress—and prioritize interventions that restore resilience while avoiding overdiagnosis or unnecessary hormone therapy.
What Holistic Therapies Support Adrenal Function and Stress Resilience?
Several holistic approaches can support adrenal resilience by addressing upstream drivers; evidence varies by therapy. Adequate protein and micronutrient intake stabilizes metabolism, adaptogens may help modulate stress responses for some people, and consistent sleep and activity plans re‑entrain circadian physiology. Clinic-based options—IV nutrient therapy or targeted detoxification—can be adjuncts for selected patients to correct deficiencies and reduce toxicant burden. Autonomic testing and patient education help tailor longer-term plans. Internal Healing and Wellness MD offers personalized evaluation and longer visits to build root-cause protocols that combine lifestyle, nutrition, and select clinic services when appropriate.
How Does Bioidentical Hormone Replacement Therapy Help Manage Stress and Cortisol Imbalance?
Bioidentical hormone replacement therapy (BHRT) uses hormones that match the molecular structure of human hormones to rebalance sex-hormone systems—changes that can indirectly improve stress resilience. BHRT does not directly lower cortisol, but correcting sex‑hormone imbalances (for example, low estrogen or testosterone) can improve sleep, energy, mood, and metabolic function, which in turn reduces HPA overactivation. BHRT is most effective when integrated into a comprehensive, personalized plan that addresses sleep, nutrition, movement, and stress management first, with hormone therapy added when clinically indicated.
The following table compares BHRT and common integrative supportive therapies by mechanism and expected outcomes:
| Therapy | Primary Mechanism | Expected Patient-Centered Outcomes |
|---|---|---|
| BHRT | Restores physiologic sex‑hormone levels | Better sleep, improved mood stability, increased energy |
| IV Nutrition Therapy | Rapid nutrient repletion and inflammation support | Faster symptom relief and improved recovery |
| Detoxification Protocols | Reduce toxicant burden to support metabolic pathways | Improved energy and lower systemic inflammation |
What Is BHRT and How Does It Address Hormonal Imbalances Related to Stress?
BHRT uses compounds that mirror human hormones to restore deficient sex hormones and improve systems like sleep architecture, mood regulation, and metabolism. By normalizing estrogen, progesterone, or testosterone when clinically appropriate, BHRT can reduce symptoms that perpetuate HPA activation—insomnia, severe fatigue, or mood instability—and thereby support lower cortisol exposure over time. Patients should receive careful hormonal assessment and ongoing monitoring; BHRT belongs within a broader, individualized strategy that emphasizes foundational lifestyle work and a balanced risk–benefit discussion.
How Do Integrative Therapies Like IV Treatments and Detoxification Support Cortisol Regulation?
Integrative therapies such as IV nutrient infusions and medically supervised detoxification can aid recovery by correcting deficiencies, reducing oxidative stress, and improving metabolic capacity—factors that ease stress-pathway burden. IV treatments deliver vitamins, minerals, and antioxidants directly to the bloodstream to support cellular energy and immune function; detox protocols aim to lower toxicant loads that interfere with endocrine signaling. These approaches are adjunctive: they can speed symptom relief and support recovery but require individualized assessment and clinical oversight. For patients interested in supervised integrative care, Internal Healing and Wellness MD (Dr. Fred Bloem) offers a root-cause evaluation and tailored protocols that may include BHRT, IV therapy, and detoxification as part of a coordinated plan to restore adrenal balance and resilience.
If symptoms are persistent or severe—unrelenting fatigue, marked weight change, refractory sleep disruption, or concerning cardiovascular signs—professional evaluation is recommended. Internal Healing and Wellness MD emphasizes a patient-centered, integrative approach focused on root causes and longer, thorough visits to develop individualized plans combining lifestyle, nutrition, and selective clinical interventions. Patients in Kensington, MD seeking assessment for cortisol imbalance, adrenal health, or personalized BHRT and supportive therapies are invited to schedule a consult to determine the safest, most effective next steps.
Frequently Asked Questions
What lifestyle changes can help manage cortisol levels effectively?
To manage cortisol effectively, focus on consistent sleep, balanced meals, regular moderate activity, and daily stress-reduction. Keep a steady sleep–wake schedule and a calming bedroom environment. Choose low‑glycemic meals with protein and fiber to prevent blood-sugar swings. Aim for 30–45 minutes of moderate exercise several times a week, and build short daily practices—breathwork, meditation, or gentle stretching—to lower physiological reactivity. These steps reliably improve stress resilience and hormonal balance for most people.
How does chronic stress affect sleep quality?
Chronic stress disrupts sleep by altering cortisol rhythms and increasing nighttime arousal. Higher evening cortisol can make it harder to fall and stay asleep, shortening total sleep time and fragmenting rest. Poor sleep then feeds back into more stress and higher cortisol, creating a vicious cycle. To break it, establish a soothing bedtime routine, reduce screen time before bed, and create a dark, cool sleeping environment. Relaxation techniques and addressing daytime stressors also help restore healthy sleep patterns.
What role do adaptogens play in managing cortisol levels?
Adaptogens are herbs that may help the body adapt to stress and modulate physiologic responses. Popular examples include ashwagandha, rhodiola, and holy basil. Some people experience reduced fatigue and improved resilience with adaptogens, but evidence varies and effects differ between individuals. Always consult a healthcare provider before starting supplements—especially if you have medical conditions or take medications—to ensure safety and appropriateness.
Can high cortisol levels lead to weight gain?
Yes. Elevated cortisol promotes gluconeogenesis and insulin resistance, which can increase blood sugar and favor fat storage, particularly in the abdominal area. Cortisol also influences appetite hormones and cravings for calorie-dense foods, making weight control more difficult. Addressing stress, stabilizing blood sugar through nutrition, and maintaining regular physical activity are key strategies to counter these effects.
What are the signs that I may need to consult a healthcare professional about cortisol levels?
If you have persistent fatigue despite sleep, significant unexplained weight changes, mood swings, memory or concentration problems, frequent infections, or ongoing sleep disturbances, consider medical evaluation. These symptoms can indicate chronic stress or adrenal dysregulation and may warrant cortisol testing and broader assessment. A clinician can recommend appropriate tests and a personalized plan to restore balance.
How does nutrition impact cortisol levels?
Nutrition strongly influences cortisol. Balanced meals with adequate protein, healthy fats, and fiber help stabilize blood sugar and reduce cortisol spikes. Low‑glycemic foods prevent rapid glucose swings that trigger cortisol release. Nutrients like magnesium and omega‑3 fatty acids support stress resilience and adrenal health. Prioritizing whole, nutrient-dense foods and limiting refined sugars and processed foods benefits cortisol regulation and overall well-being.
Conclusion
Cortisol plays a vital role in how your body responds to stress. By prioritizing sleep, stable nutrition, appropriate movement, and regular stress-reduction, you can lower excessive cortisol exposure and build greater resilience. The steps outlined here translate physiology into practical actions that improve energy, mood, and long-term health. For tailored guidance and supervised options, consider scheduling a consultation with our team to create a personalized plan.



