
Chiropractic Care for Spinal Health — How It Helps, When It’s Right, and Holistic Alternatives
Chiropractic care uses hands-on, non-surgical techniques to protect and restore spinal health — improving alignment, mobility, and nervous system function. This guide walks you through how chiropractic care can relieve back pain and improve posture, where it fits inside a holistic care plan, and which regenerative and integrative options exist if tissue-level repair is needed. Many people live with persistent low back pain, sciatica, or stiffness that limits activity and quality of life. Knowing how spinal manipulation works, what realistic results look like, and how it pairs with rehabilitation and regenerative therapies helps set clear expectations. We cover the main benefits of spinal adjustments, how they influence alignment and nerve function, posture strategies you can use, and a practical comparison between manual care and biologic therapies. You’ll also find what to expect during a clinical consultation and how clinics like Internal Healing and Wellness MD blend regenerative and holistic options into patient-focused plans so you can make an informed decision for long-term spinal wellness.
What Are the Key Benefits of Chiropractic Spinal Adjustments?
Spinal adjustments are hands-on treatments designed to restore normal joint motion, ease soft-tissue tension, and reduce pain by improving vertebral alignment. Techniques range from targeted, quick thrusts to gentler mobilizations aimed at a specific spinal segment. These interventions can restore range of motion and lower nociceptive signals coming from irritated joints. Many patients notice measurable pain relief, better mobility, and improved function after a course of care — especially with acute or subacute low back pain. Current clinical guidance supports spinal manipulation as part of conservative, non-surgical pain management when delivered by trained clinicians alongside exercise and education.
Common advantages of chiropractic adjustments include:
- Reduced pain in acute and chronic low back conditions through decreased joint and muscle irritation.
- Improved spinal alignment and segmental mobility that supports everyday movement.
- Better nerve-related symptoms by lowering mechanical compression and local inflammation.
- Short-term functional gains and quality-of-life improvements that can speed rehabilitation.
These gains last longest when adjustments are combined with active rehabilitation and sensible lifestyle changes. The next section explains the mechanics behind alignment and mobility improvements.
How Do Chiropractic Adjustments Improve Spinal Alignment and Mobility?
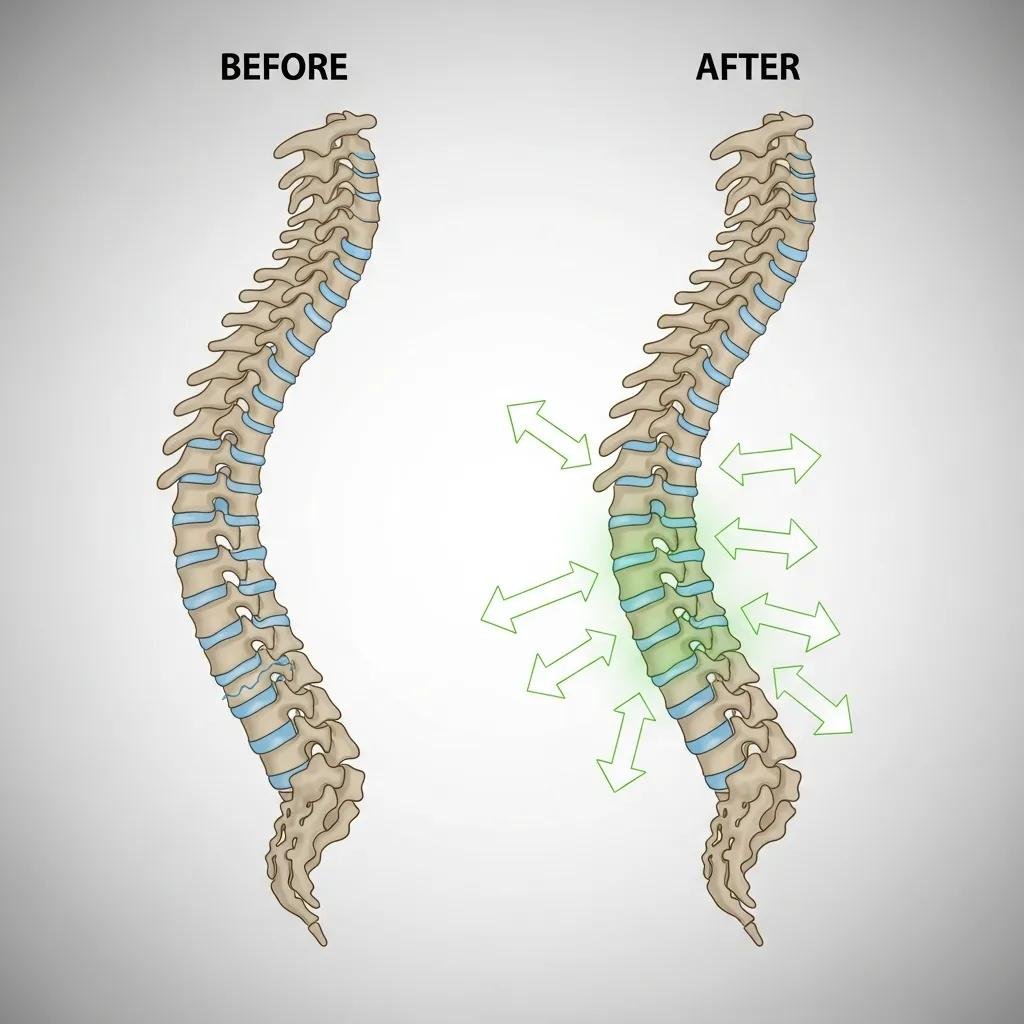
Adjustments apply controlled forces to vertebrae to free joint adhesions, normalize joint capsule mechanics, and correct abnormal movement patterns. That mechanical effect often brings immediate increases in range of motion as paraspinal muscles relax and proprioception improves. On a physiologic level, manipulation can lower intra‑articular pressure, activate mechanoreceptors that dampen pain pathways, and encourage synovial fluid movement in the facet joints. Whether treating acute stiffness after a lift or long-standing hypomobility from poor posture, the goal is to restore more functional motion.
Research and clinical experience show that repeated, targeted adjustments combined with active exercises deliver more durable mobility gains than passive care alone. Practically, patients often notice easier bending, less stiffness, and improved walking tolerance within days to weeks, while ongoing treatment addresses persistent movement patterns. That sets up the next topic: how better alignment affects nerve function and pain perception.
In What Ways Does Chiropractic Care Enhance Nerve Function and Reduce Back Pain?
Chiropractic care can improve nerve function indirectly by removing mechanical irritants and directly through reflex changes that modulate pain. When spinal segments move more normally, compression and inflammatory signaling around nerve roots tend to decrease — which can ease radicular pain and numbness. Manipulation also stimulates large mechanoreceptors that inhibit nociceptive transmission at the spinal cord level, offering relatively rapid pain relief for some patients. These changes often translate into better sleep, steadier gait, and greater ability to participate in rehabilitation.
Safety and limitations matter: chiropractic is not appropriate when clear red flags are present, such as progressive neurologic loss, unstable fractures, or certain vascular conditions. Thoughtful diagnostic evaluation, shared decision‑making, and imaging when indicated keep care safe and effective. With those safeguards, chiropractic remains a validated non-surgical option for many causes of low back pain and sciatica and complements other conservative measures. The next section covers how chiropractic supports posture and long-term spinal health.
How Does Chiropractic Care Support Posture and Overall Spinal Health?
Chiropractic care supports posture by correcting biomechanical imbalances, releasing soft‑tissue restrictions, and teaching movement strategies that reduce repetitive stress on the spine. Common postural problems — like forward head carriage or excess lumbar flexion — create uneven loading on discs, facet joints, and paraspinal muscles, accelerating wear and pain. Through targeted assessment, adjustments, and soft‑tissue techniques, clinicians can restore more balanced alignment and improve postural control. When paired with strengthening and ergonomic changes, alignment work helps slow degenerative processes.
Durable postural improvement usually combines hands‑on care with home exercises and workplace adjustments. Strengthening the core and scapular stabilizers, retraining motor patterns, and changing daily habits reduce relapse risk. The following subsection outlines the specific role of chiropractic within a multimodal postural rehabilitation plan.
What Is the Role of Chiropractic Treatment in Correcting Postural Issues?
Postural correction begins with a thorough assessment to identify spinal deviations, muscle imbalances, and habitual movement patterns. Treatment blends targeted adjustments to restore joint position, soft‑tissue work to ease fascial tension, and neuromuscular retraining exercises to reinforce better movement. Care is typically sequenced: adjustment sessions paired with progressive exercise prescriptions and ergonomic coaching to address sitting, repetitive tasks, and other daily stressors. This multimodal approach helps patients form sustainable postural habits that protect the spine.
Progress is tracked with objective measures — posture photos, range‑of‑motion tests, and functional assessments — so clinicians can adapt the plan. When posture improves and strength and flexibility increase, patients usually report less mechanical pain and greater endurance. Those biomechanical benefits support long‑term spinal health, which the next subsection explains.
How Does Improved Posture Contribute to Long-Term Spinal Wellness?
Better posture reduces abnormal loading on vertebrae, discs, and facet joints, lowering the pace of degenerative changes and the risk of recurrent pain. Improved alignment also supports breathing mechanics and core stability, helping daily function and athletic performance. Long‑term spinal wellness relies on movement variability — avoiding prolonged static positions — and on maintaining strength in stabilizing muscles so forces are distributed evenly. Preventive posture work can therefore reduce cumulative risk for disc problems and chronic pain.
Sustained postural control also helps preserve foraminal space and reduce intermittent nerve root irritation. When posture work is combined with periodic maintenance care and an active lifestyle, the chance of relapse falls. With that context, many patients ask how chiropractic care compares with regenerative joint therapies — the next section addresses that comparison.
What Are the Differences Between Chiropractic Care and Regenerative Joint Therapies?
Chiropractic care and regenerative joint therapies take different but potentially complementary approaches to non‑surgical spinal care. Chiropractic prioritizes mechanical correction of spinal segments and neuromuscular balance; regenerative therapies aim to change tissue biology and promote repair. Key contrasts include mechanism (mechanical realignment vs. biologic repair), timeline (immediate mechanical change vs. gradual tissue remodeling), and typical indications (hypomobility and soft‑tissue dysfunction vs. degenerative joint disease and tissue loss). Understanding these differences helps patients and clinicians choose a pathway — or combine approaches — based on the specific spinal diagnosis.
| Approach | Mechanism | Typical Indications |
|---|---|---|
| Chiropractic adjustments | Mechanical correction of joint position and neuromuscular inhibition | Acute/subacute back pain, joint hypomobility, muscle spasm |
| Platelet-Rich Plasma (PRP) / Prolozone / Laser intra-articular | Biologic stimulation of tissue repair, reduced inflammation, growth factor delivery | Degenerative facet disease, localized joint degeneration, refractory focal pain |
| PEMF / TruDOSE regenerative technologies | Energy-based modulation of cellular activity and inflammation | Chronic pain states with tissue-level degeneration and healing deficits |
In short: chiropractic often delivers faster biomechanical relief, while regenerative therapies aim to change tissue biology over weeks to months. For many patients, a combined pathway — mechanical optimization followed by biologic support — provides the best chance of lasting improvement.
Preliminary clinical evidence supports combination strategies for selected patients. At Internal Healing and Wellness MD we offer regenerative options — including PRP, Prolozone, PEMF, intra‑articular laser, and TruDOSE — as complements or alternatives when tissue repair is the primary goal. The next subsection explains how regenerative therapies can be integrated with or substituted for manual care, depending on diagnosis and goals.
How Do Regenerative Therapies Complement or Serve as Alternatives to Chiropractic Adjustments?
Regenerative therapies address the biological factors behind chronic joint pain while adjustments address alignment and movement restrictions. For example, a patient with facet arthropathy may receive adjustments to improve mobility and reduce pain immediately, then pursue PRP or Prolozone injections to support longer‑term tissue healing. Conversely, when imaging shows focal degeneration unlikely to respond to manipulation alone, regenerative treatments may be considered earlier in the care pathway.
Most clinicians follow a conservative‑to‑biologic sequence: start with rehab and manual care, then escalate to regenerative modalities if structural degeneration or persistent symptoms remain. Safety, the underlying pathology, and patient preferences guide decision making.
What Conditions Can Be Addressed by Regenerative Joint Therapies for Spinal Health?
Regenerative injections and energy‑based therapies are useful for localized spinal problems where tissue degeneration or chronic inflammation play a central role. Typical targets include facet arthropathy, focal degenerative changes of small spinal joints, and chronic paraspinal soft‑tissue injuries that have not improved with standard conservative care. Expectations should be realistic: regenerative treatments aim to reduce symptoms and support tissue recovery, not guarantee full structural reversal.
Appropriate patient selection requires imaging, identification of contraindications, and multidisciplinary evaluation. When used properly, regenerative therapies can extend the benefits of mechanical care and support longer‑lasting functional gains.
How Can Holistic and Integrative Approaches Enhance Spinal Health Beyond Chiropractic?

Holistic and integrative strategies boost spinal recovery by addressing systemic drivers — chronic inflammation, metabolic dysfunction, and hormonal imbalances — that affect tissue repair and pain sensitivity. Treating the spine alone can miss contributors like poor nutrition, inadequate sleep, or metabolic issues that impede healing. Integrative care combines biologic treatments, targeted nutrition, exercise, and metabolic optimization to lower inflammatory burden, improve tissue quality, and support rehabilitation. A systems‑level approach increases the odds of sustained improvement and reduces recurrence.
Core pillars of integrative spinal care include lifestyle modification, functional medicine assessment, hormonal balance, and adjunct therapies that support cellular recovery. Key components used in comprehensive spinal care include:
- Nutrition and anti‑inflammatory eating plans to lower systemic inflammation and support tissue repair.
- Functional assessments and metabolic optimization to uncover contributors like insulin resistance or micronutrient gaps.
- Adjunctive tools such as IV nutrient support, hormone optimization, and targeted regenerative therapies to accelerate healing.
These pillars work together: improved nutrition and metabolic health make regenerative and manual therapies more effective. The table below summarizes common integrative services and how they support spinal health.
| Service | Goal / Mechanism | Benefit for Spinal Health |
|---|---|---|
| IV nutrient therapy | Rapid delivery of vitamins and antioxidants to support cellular repair | Reduces oxidative stress and supports recovery after procedures |
| Bioidentical hormone replacement | Restores hormonal balance that influences inflammation and tissue repair | Improves healing capacity and may reduce chronic pain drivers |
| Nutrition and weight optimization | Lowers systemic inflammatory mediators and decreases mechanical load | Reduces degenerative stress on spinal structures |
When combined into a personalized protocol, these services address root causes rather than only masking symptoms. Internal Healing and Wellness MD emphasizes individualized plans that blend functional medicine, hormone balance, nutrition, IV therapies, and regenerative joint care to create more durable spinal outcomes while keeping chiropractic care as a core mechanical strategy.
What Is the Importance of Addressing Root Causes in Back Pain Management?
Treating root causes shifts care from symptom control to lasting recovery. Systemic factors like chronic inflammation, metabolic syndrome, hormonal imbalance, and lifestyle choices can drive pain chronification and impair tissue healing. By reducing inflammatory mediators and optimizing metabolic health, clinicians improve the biological environment for repair and lower the chance of recurrence. This approach often reduces reliance on symptomatic medications and supports sustained functional gains.
Root‑cause interventions include targeted nutritional changes, anti‑inflammatory strategies, metabolic optimization, and hormonal evaluation where appropriate. Addressing these factors amplifies the effect of mechanical and regenerative interventions and creates synergistic improvements.
How Do Personalized Treatment Protocols Improve Outcomes for Spinal Health?
Personalized protocols align diagnostic findings, patient goals, and evidence‑based interventions into a flexible plan that adapts to response. Key steps include a detailed history, targeted imaging or labs when needed, baseline pain and function measures, and shared decision‑making around sequencing conservative, regenerative, and integrative modalities. Personalization ensures that patients with largely mechanical dysfunction focus on rehabilitation and adjustments, while those with tissue degeneration receive regenerative support alongside metabolic and hormonal optimization.
Progress is tracked with objective measures such as pain scales and functional tests so care can be adjusted. This iterative approach improves adherence, optimizes resource use, and produces better pain relief and functional restoration over time.
What Should Patients Expect During a Consultation for Spinal Health at Internal Healing and Wellness MD?
A spinal health consultation at Internal Healing and Wellness MD starts with a comprehensive intake that maps symptoms, prior care, and functional limitations to form a working diagnosis. The clinician performs a focused physical and neurologic exam to assess spinal mobility, nerve function, posture, and movement patterns, and orders imaging or lab work when indicated to clarify structural or systemic contributors. After synthesizing findings, we review conservative options (including chiropractic), regenerative possibilities, and integrative strategies — aligning recommendations with your goals and safety considerations.
Our consultation process emphasizes shared decision‑making and an individualized plan that sequences rehabilitation, adjustments, and regenerative or integrative therapies as appropriate. Patients receive clear goals, realistic timeframes, and follow‑up intervals to monitor progress. The table below summarizes common consultation components so you know what to expect.
| Component | Purpose | Typical Outcome |
|---|---|---|
| History & symptom mapping | Identify pain patterns, triggers, and prior interventions | Clarifies diagnostic hypothesis and treatment priorities |
| Physical and neurologic exam | Assess mobility, strength, and nerve function | Objective baseline to guide manual and rehabilitative care |
| Diagnostic planning & shared decision-making | Determine imaging/lab needs and agree on therapy sequence | Personalized plan with measurable goals and follow-up |
How Is a Personalized Treatment Plan Developed for Back Pain and Spinal Issues?
A personalized plan grows from the diagnostic inputs — history, exam, imaging, and relevant labs — combined with your goals and safety priorities. We generally prioritize conservative measures like targeted exercise, posture correction, and manual therapy, reserving regenerative interventions for persistent structural degeneration or failed conservative care. The plan outlines sequencing, expected timelines, improvement benchmarks, and contingency steps if progress stalls. Shared decision‑making ensures you understand the options and consent to the proposed path.
Typical pathways include a rehabilitation‑first model for mechanical problems, or a combined approach where initial mechanical optimization is followed by PRP or Prolozone to address focal degeneration. Standard outcome measures and scheduled reassessments help refine the plan over time.
What Are Patient Success Stories Demonstrating the Effectiveness of Holistic Spinal Care?
Here are anonymized examples that illustrate common outcomes from integrated care. One patient, a middle‑aged office worker with chronic low back stiffness, combined manual adjustments, a structured exercise program, and targeted anti‑inflammatory nutrition to regain full work capacity in about three months.
Another patient with focal facet degeneration completed a course of chiropractic mobilization and then received PRP injections, reporting progressive pain reduction and improved activity tolerance over a twelve‑week period.
A third patient with recurrent radicular symptoms improved markedly after combined neuromuscular rehabilitation and metabolic optimization.
These cases show that multimodal care — pairing mechanical, biologic, and systemic interventions — can deliver meaningful improvements for the right patients. Success depends on accurate diagnosis, realistic expectations, and adherence to a personalized plan.
Why Choose Dr. Fred Bloem’s Clinic for Holistic Spinal Health and Pain Relief?
Internal Healing and Wellness MD, led by Dr. Fred Bloem, focuses on integrative, root‑cause approaches to spinal health and non‑surgical pain relief. Our model blends regenerative joint therapies with supportive integrative services, emphasizes longer visits for education, and builds personalized protocols that prioritize function and durable outcomes. We aim to provide a coordinated plan that may include conservative manual care, targeted regenerative options, and metabolic or hormonal optimization when indicated.
- Longer visits that allow in‑depth history‑taking and patient education about spinal health.
- A menu of regenerative modalities — PRP, Prolozone, PEMF, intra‑articular laser, and TruDOSE — available as complements to conservative care.
- An integrative approach that pairs regenerative treatments with nutrition, IV therapies, and hormone optimization to address root causes.
| Clinic Strength | Characteristic | Patient Benefit |
|---|---|---|
| Regenerative modalities | PRP, Prolozone, PEMF, laser, TruDOSE | Tissue-focused treatment options beyond symptom relief |
| Integrative services | Nutrition, IV therapy, hormone optimization | Systemic support that promotes healing and lowers recurrence |
| Patient-centered process | Longer visits and focused education | Clear expectations, better adherence, improved outcomes |
What Unique Value Propositions Differentiate Internal Healing and Wellness MD?
We differentiate our clinic through a root‑cause philosophy, extended appointment times for detailed evaluation, and an array of regenerative and integrative options beyond typical symptom‑focused care. That combination lets clinicians design individualized plans that sequence conservative, biologic, and systemic interventions based on objective findings and patient priorities. Education is central — we help patients participate actively in their recovery so lifestyle changes and rehabilitation stick.
How Does the Clinic Integrate Regenerative Medicine with Holistic Practices for Spinal Wellness?
We usually sequence care so regenerative injections or energy‑based therapies follow a phase of mechanical optimization and targeted rehabilitation, unless imaging or clinical urgency points to earlier biologic intervention. For example, a patient may complete posture correction, core stabilization, and manual therapy to resolve movement restrictions before receiving PRP for persistent facet degeneration. At the same time, nutrition counseling, IV nutrient support, and hormone evaluation improve the body’s capacity to heal and reduce inflammation, which can enhance regenerative outcomes.
Outcomes are tracked with baseline and follow‑up functional tests and pain scores to confirm treatment effect and guide maintenance. This sequence — mechanical optimization, biologic repair, and systemic support — creates a comprehensive pathway for lasting spinal wellness under Dr. Bloem’s care model.
Frequently Asked Questions
1. What types of conditions can chiropractic care effectively treat?
Chiropractic care addresses a wide range of musculoskeletal complaints, especially those involving the spine. Typical issues include acute and chronic low back pain, neck pain, headaches, sciatica, and joint dysfunction. It can also assist with sports injuries, repetitive strain complaints, and postural problems. While primarily focused on mechanical dysfunction, chiropractic care supports overall function and mobility and is often part of a broader non‑surgical strategy.
2. How often should one visit a chiropractor for optimal results?
Visit frequency depends on your condition, its severity, and your goals. Acute problems may require more frequent visits initially (often 1–3 times per week) to control pain and establish a treatment plan. As you improve, visits typically taper to biweekly or monthly maintenance. Your clinician will recommend a schedule and adjust it based on progress and goals.
3. Are there any risks associated with chiropractic adjustments?
When delivered by trained professionals, chiropractic adjustments are generally safe. Common transient effects include soreness, stiffness, or mild discomfort after treatment. Rare but more serious complications — such as nerve injury or vascular events — are uncommon and typically related to specific preexisting conditions. A full medical history, appropriate screening, and shared decision‑making help minimize risks.
4. Can chiropractic care be combined with other treatments?
Absolutely. Chiropractic care often works best as part of a multidisciplinary approach alongside physical therapy, massage, acupuncture, and nutritional guidance. Coordinated care addresses multiple contributors to pain and function and can speed recovery while reducing the chance of relapse.
5. What lifestyle changes can support chiropractic treatment?
Supportive lifestyle changes include regular exercise focused on core strength and flexibility, maintaining a healthy weight, and improving workplace ergonomics to avoid poor posture. Good sleep habits and supportive bedding help spinal alignment during rest. An anti‑inflammatory diet also supports recovery and overall health.
6. How does chiropractic care fit into a holistic health approach?
Chiropractic care is a core component of holistic health because it addresses spinal alignment and nervous system function, which affect overall well‑being. When combined with nutrition, stress management, exercise, and systemic optimization, chiropractic care helps treat root causes and supports long‑term wellness.
7. What should I expect during my first chiropractic visit?
Your first visit will include a thorough medical history and a focused physical exam to assess posture, spinal alignment, and range of motion. The clinician may order diagnostic tests if needed. Based on findings, you’ll receive a personalized plan and the chance to ask questions so you understand the approach and goals.
Conclusion
Chiropractic care can play an important role in spinal health — offering pain relief, improved mobility, and positive effects on nerve function. Paired with rehabilitation, thoughtful lifestyle changes, and, when appropriate, regenerative or integrative therapies, it becomes part of a durable, patient‑centered plan. If you’re exploring options, Internal Healing and Wellness MD can help you weigh chiropractic care against regenerative and systemic approaches to find the right path for long‑term spinal wellness. Take the next step by scheduling a consultation with our team to discuss a personalized plan.



